Unique Cannabis Flavonoids and Their Medical Applications
Cannabis sativa, renowned for its medicinal versatility, is a complex plant with a broad spectrum of bioactive compounds. Beyond the widely studied cannabinoids like tetrahydrocannabinol (THC) and cannabidiol (CBD), cannabis contains a range of flavonoids that have garnered significant attention for their therapeutic potential. Flavonoids are polyphenolic compounds that contribute to the plant’s pigmentation, aroma, and health benefits. While flavonoids are present in many plant species, cannabis is unique in containing certain flavonoids, such as cannflavins, which exhibit remarkable pharmacological properties. This analysis provides an in-depth exploration of the medical applications of cannabis flavonoids, focusing exclusively on their therapeutic effects, excluding recreational aspects or methods of consumption.
1. Flavonoids in Cannabis: A Unique Chemical Spectrum
Flavonoids are secondary metabolites that make up approximately 10% of the bioactive substances in cannabis. They serve essential roles in plant defense, UV protection, and pollination. In the human body, these compounds interact with biological pathways to produce anti-inflammatory, antioxidant, antimicrobial, and anticancer effects. Over 20 flavonoids have been identified in cannabis, with some being exclusive to the plant.
1.1 Notable Flavonoids in Cannabis
- Cannflavins A, B, and C: Unique to cannabis, these compounds are potent anti-inflammatory agents.
- Apigenin: Known for its anxiolytic, anti-cancer, and anti-inflammatory effects.
- Quercetin: A powerful antioxidant and antiviral agent.
- Kaempferol: Demonstrates anti-inflammatory and anticancer properties.
The pharmacological diversity of these flavonoids positions them as promising candidates for addressing various medical conditions. By targeting specific molecular pathways, these compounds offer therapeutic benefits that complement traditional medications.
2. Cannflavins: Cannabis-Specific Anti-Inflammatory Compounds
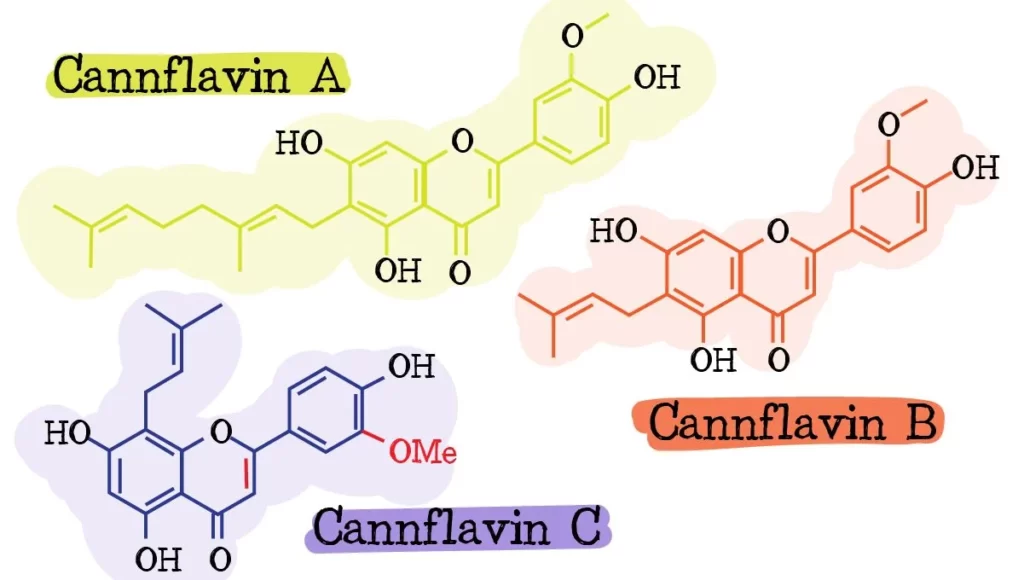
Cannflavins A, B, and C are unique flavonoids that set cannabis apart from other medicinal plants. These compounds are particularly noteworthy for their potent anti-inflammatory properties. Unlike non-steroidal anti-inflammatory drugs (NSAIDs), which primarily inhibit the COX-1 and COX-2 enzymes, cannflavins act through a dual mechanism targeting prostaglandins and leukotrienes.
2.1 Mechanism of Action
Cannflavins inhibit the production of prostaglandin E2 (PGE2), a key mediator of inflammation, while also modulating the lipoxygenase pathway. This dual inhibition results in significantly reduced inflammation without the gastrointestinal side effects commonly associated with NSAIDs.
2.2 Medical Applications
Chronic Inflammatory Diseases
Chronic inflammation underlies a wide range of diseases, including rheumatoid arthritis, inflammatory bowel disease (IBD), and osteoarthritis. Cannflavins have shown potential to:
- Reduce swelling and discomfort in diseases such as rheumatoid arthritis.
- Protect the gastrointestinal lining while addressing inflammation in diseases such as Crohn’s disease and ulcerative colitis.
Neuroinflammatory Disorders
Neurodegenerative diseases like Alzheimer’s and Parkinson’s are characterized by persistent inflammation in the central nervous system. Cannflavins may slow disease progression by reducing neuroinflammation, protecting neurons, and improving cognitive function.
Post-Traumatic Inflammation
Cannflavins could be particularly beneficial in reducing inflammation associated with acute injuries, post-surgical recovery, or sports-related trauma. Their targeted action minimizes systemic side effects, making them ideal for long-term use.
3. Apigenin: A Multifaceted Flavonoid
Apigenin, a flavonoid commonly found in parsley, chamomile, and cannabis, has garnered attention for its diverse pharmacological activities. It is particularly effective in reducing anxiety, inflammation, and cancer cell proliferation.
3.1 Anti-Cancer Properties of Apigenin
Apigenin has demonstrated the ability to suppress cancer cell growth through multiple pathways, including:
- Induction of Apoptosis: Apigenin triggers programmed cell death by downregulating anti-apoptotic proteins such as Bcl-2.
- Inhibition of Metastasis: By blocking the PI3K/Akt signaling pathway, apigenin prevents cancer cells from spreading to other parts of the body.
- Antioxidant Effects: Its ability to neutralize free radicals reduces oxidative stress, a critical factor in cancer progression.
Medical Applications:
- Treatment of Various Cancers:
- Preclinical studies indicate efficacy against breast, prostate, and lung cancers.
- Apigenin enhances the effectiveness of chemotherapy drugs, reducing their required dosage and associated toxicity.
- Preventive Oncology:
- As an antioxidant, apigenin may prevent the genetic mutations that initiate cancer development, making it valuable for individuals at high risk of developing cancer.
3.2 Anxiolytic Effects of Apigenin
Apigenin binds to benzodiazepine receptors on GABA-A, a neurotransmitter system associated with relaxation and anxiety reduction. Unlike conventional anxiolytics, apigenin provides a calming effect without causing sedation or dependence.
Medical Applications:
- Generalized Anxiety Disorder (GAD):
- Apigenin offers a natural alternative to traditional anxiety medications, addressing symptoms without causing cognitive impairment or addiction.
- Sleep Disorders:
- By promoting relaxation, apigenin may improve sleep quality in patients with insomnia, particularly those with stress-induced sleep disturbances.
4. Quercetin: An Antioxidant and Antiviral Powerhouse
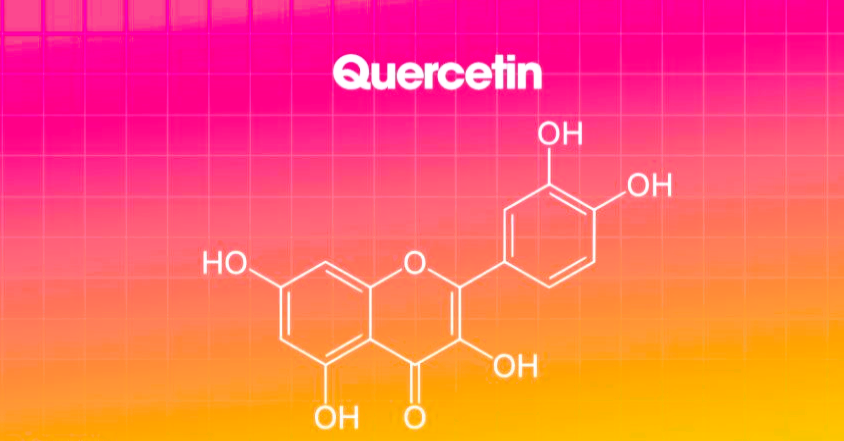
Quercetin is a flavonoid abundant in cannabis and other plant-based foods. It is well-regarded for its antioxidant, anti-inflammatory, and antiviral properties. These effects make quercetin a versatile compound in the prevention and treatment of chronic diseases.
4.1 Antioxidant Effects
Quercetin combats oxidative stress by scavenging free radicals and reducing lipid peroxidation. This protective action is crucial for preventing cellular damage and slowing the progression of age-related diseases.
Medical Applications:
- Cardiovascular Protection:
- Quercetin reduces oxidative damage to the vascular endothelium, preventing the development of atherosclerosis.
- It also lowers blood pressure by enhancing nitric oxide availability, improving vascular function.
- Neurodegenerative Disease Prevention:
- Oxidative stress is a major factor in conditions like Alzheimer’s and Parkinson’s disease. Quercetin protects neurons from damage, potentially slowing disease progression.
4.2 Antiviral Properties
Quercetin has shown broad-spectrum antiviral activity, making it a valuable compound for treating viral infections. Its mechanisms include inhibiting viral replication, blocking viral entry into host cells, and modulating immune responses.
Medical Applications:
- Treatment of Viral Infections:
- Quercetin has demonstrated efficacy against influenza, herpes simplex, and potentially SARS-CoV-2, the virus responsible for COVID-19.
- Its immune-modulating properties enhance the body’s ability to fight infections while reducing the risk of cytokine storms.
- Immune System Support:
- As an immunomodulator, quercetin balances immune responses, making it beneficial for autoimmune conditions or during viral outbreaks.
5. Kaempferol: Anti-Inflammatory and Anticancer Effects
Kaempferol is a flavonoid present in cannabis that exhibits significant antioxidant, anti-inflammatory, and anticancer properties. Its broad therapeutic potential makes it an essential compound for medical research.
5.1 Anti-Cancer Properties of Kaempferol
Kaempferol inhibits key processes involved in cancer development, including:
- Angiogenesis: It suppresses the formation of new blood vessels that feed tumors, effectively starving them of nutrients.
- Induction of Apoptosis: Like apigenin, kaempferol promotes programmed cell death in cancer cells.
Medical Applications:
- Treatment of Advanced Cancers:
- Kaempferol has shown promise against difficult-to-treat cancers, such as pancreatic and liver cancers.
- When used alongside chemotherapy, it reduces drug resistance and enhances treatment efficacy.
- Cancer Prevention:
- By reducing oxidative stress and chronic inflammation, kaempferol may prevent the initiation of cancer in at-risk populations.
5.2 Anti-Inflammatory Effects
Kaempferol inhibits the production of inflammatory mediators, including cytokines and COX-2 enzymes. This makes it valuable for managing chronic inflammatory conditions.
Medical Applications:
- Autoimmune Diseases:
- Conditions such as lupus and multiple sclerosis may benefit from kaempferol’s ability to modulate immune responses and reduce systemic inflammation.
- Chronic Pain Management:
- Kaempferol’s anti-inflammatory effects can complement pain relief strategies, reducing reliance on opioids or NSAIDs.
6. Synergistic Effects: Flavonoids in Combination with Cannabinoids
One of the unique features of cannabis is the “entourage effect,” where flavonoids, cannabinoids, and terpenes interact synergistically to enhance therapeutic outcomes. This effect underscores the importance of whole-plant medicine in maximizing the medical benefits of cannabis.
6.1 Enhanced Anti-Inflammatory Effects
Cannflavins, when combined with CBD, provide stronger anti-inflammatory effects than either compound alone. This combination may be particularly effective in treating autoimmune diseases, chronic pain, and neuroinflammation.
6.2 Amplified Antioxidant Protection
The antioxidant effects of quercetin and kaempferol are enhanced by their interaction with cannabinoids, offering superior protection against oxidative damage.
Medical Applications:
- Comprehensive Cancer Treatment:
- The combination of flavonoids and cannabinoids targets multiple cancer pathways, increasing the likelihood of treatment success.
- This approach reduces the required dose of chemotherapy drugs, minimizing adverse side effects.
- Management of Complex Disorders:
- Diseases involving inflammation, oxidative stress, and immune dysfunction—such as multiple sclerosis—benefit from the multifaceted effects of cannabis compounds.
Restrictions on Cannabis Components in the Medical Field: Ensuring Safety and Efficacy

The use of cannabis and its components in medicine has grown significantly in recent years, driven by mounting evidence of its therapeutic benefits. However, the integration of cannabis-based treatments into mainstream medical practice is not without challenges. One of the primary concerns is ensuring patient safety, particularly regarding the psychoactive effects of tetrahydrocannabinol (THC). Regulatory frameworks and clinical guidelines have imposed restrictions on cannabis components, focusing on their use as a last resort and closely monitoring THC levels to prevent psychoactivity. This article explores these restrictions and their implications for medical practice.
1. Cannabis as a Last-Resort Treatment
In many countries, cannabis-based medications are reserved for patients who have exhausted conventional treatments. This restriction ensures that cannabis is used only in cases where standard therapies have failed or are unsuitable.
1.1 Guidelines for Last-Resort Usage
Cannabis medications are typically prescribed for conditions such as chronic pain, epilepsy, multiple sclerosis, and chemotherapy-induced nausea and vomiting. Medical professionals must demonstrate that:
- Conventional Options Have Been Tried: Patients must undergo established treatments before cannabis-based options are considered.
- Documented Ineffectiveness or Side Effects: Evidence must show that other treatments were either ineffective or caused intolerable side effects.
1.2 Ethical Considerations
The use of cannabis as a last resort reflects an ethical commitment to prioritizing evidence-based and well-studied therapies. This approach minimizes potential risks associated with cannabis components, particularly those that may have long-term or unpredictable effects on patients.
2. Monitoring THC Levels to Prevent Psychoactivity
Tetrahydrocannabinol (THC) is the primary psychoactive component in cannabis, and its effects on cognition and behavior pose challenges in medical contexts. Monitoring and controlling THC levels in cannabis-based medications is critical to ensuring patient safety and therapeutic efficacy.
2.1 Regulatory THC Limits
Most medical cannabis products are subject to strict regulations regarding their THC content. Although these restrictions differ by jurisdiction, they usually consist of:
- Low-THC Thresholds: In many regions, medical cannabis products must contain less than 0.3–1% THC to be legally prescribed.
- CBD-THC Ratios: Cannabidiol (CBD), a non-psychoactive compound, is often combined with THC to mitigate its psychoactive effects. High CBD-to-THC ratios are preferred for medical use.
2.2 Ensuring Non-Psychoactive Effects
To prevent psychoactive side effects, medical professionals and pharmaceutical manufacturers implement several strategies:
- Microdosing THC: Patients receive minimal THC doses, just enough to achieve therapeutic benefits without causing intoxication.
- Isolated Cannabinoids: Products containing isolated CBD or other non-psychoactive cannabinoids are increasingly favored for their safety profiles.
2.3 Monitoring in Vulnerable Populations
Certain groups, such as children, the elderly, and individuals with psychiatric disorders, are particularly sensitive to THC. For these populations:
- Strict THC-Free Formulations: Many medications are formulated to exclude THC entirely.
- Ongoing Monitoring: Patients undergo regular evaluations to assess any cognitive or behavioral changes, ensuring their safety.
3. Restricting Components to Prevent Abuse and Misuse
The potential for cannabis products to be misused or abused necessitates additional restrictions on their distribution and prescription. These measures aim to maintain the integrity of medical cannabis as a legitimate therapeutic option.
3.1 Prescription Controls
To prevent inappropriate use, cannabis medications are tightly controlled through prescription-only access. Physicians prescribing these treatments must:
- Undergo Specialized Training: Medical professionals are required to complete certifications or training in cannabis therapeutics to ensure informed prescribing.
- Follow Patient-Specific Protocols: Prescriptions must be tailored to individual patient needs, taking into account their medical history and potential risk factors.
3.2 Restrictions on Non-Medical Components
Flavonoids, terpenes, and other non-psychoactive components of cannabis are also regulated to ensure consistency and quality. While these compounds do not cause intoxication, their interactions with cannabinoids can influence therapeutic outcomes. As such:
- Standardized Formulations: Products must adhere to standardized concentrations of active ingredients to avoid variability in effects.
- Batch Testing: Routine testing of products ensures they meet regulatory standards and do not contain contaminants or excess THC.
4. Surveillance and Post-Market Monitoring
The use of cannabis-based medications is subject to ongoing surveillance to track patient outcomes and potential adverse effects. This post-market monitoring ensures that the safety and efficacy of these treatments are continually assessed.
4.1 Patient Monitoring Systems
Healthcare providers often use patient registries and electronic health records to track the impact of cannabis medications. This data helps identify:
- Adverse Effects: Symptoms such as dizziness, anxiety, or cognitive impairment can be flagged and managed promptly.
- Long-Term Outcomes: Chronic use of cannabis-based treatments is monitored to detect any unforeseen health impacts.
4.2 Pharmacovigilance Programs
Regulatory agencies require pharmaceutical companies to implement robust pharmacovigilance systems for cannabis products. These programs involve:
- Reporting Requirements: Physicians and patients must report any adverse events to regulatory bodies.
- Real-World Evidence Collection: Data from diverse patient populations is analyzed to refine treatment guidelines and improve safety protocols.
5. Challenges and Future Directions
Despite these restrictions, challenges remain in integrating cannabis components into mainstream medical practice. Key issues include:
5.1 Balancing Access and Safety
While restrictions ensure patient safety, they may limit access for individuals who could benefit from cannabis-based treatments. Striking a balance between safeguarding public health and meeting patient needs is a critical challenge for policymakers.
5.2 Advancing Research
Limited research on cannabis components, particularly THC and its interactions with other cannabinoids, hampers the development of optimized medical formulations. Increased funding and regulatory support for clinical trials are essential to address this knowledge gap.
5.3 Education and Awareness
Healthcare professionals and patients alike require greater education on the risks and benefits of cannabis medications. Training programs, patient education campaigns, and clear labeling of products can enhance informed decision-making.
Conclusion
The medical use of cannabis and its components, including flavonoids, cannabinoids, and terpenes, presents immense therapeutic potential for treating a variety of conditions, including chronic inflammation, cancer, neurodegenerative disorders, and viral infections. However, the integration of cannabis into medical practice requires a careful and balanced approach to address safety, efficacy, and ethical concerns.
Cannabis flavonoids, such as cannflavins, apigenin, quercetin, and kaempferol, demonstrate unique pharmacological properties. Their anti-inflammatory, antioxidant, anticancer, and antiviral effects position them as promising candidates for targeted therapies. The “entourage effect,” where flavonoids interact synergistically with cannabinoids like CBD, enhances their therapeutic benefits, making whole-plant medicine an important area of focus. This synergy supports the development of personalized treatment approaches for complex conditions.
To ensure safe application, cannabis-based medications are often reserved as a last resort, particularly for patients who have exhausted conventional therapies. This limitation reflects an ethical commitment to prioritize well-researched treatments while offering hope for those with otherwise intractable conditions. Monitoring and controlling THC levels in these medications is critical to avoiding psychoactive effects, particularly for vulnerable populations like children, the elderly, and individuals with psychiatric disorders. Low-THC or THC-free formulations, combined with rigorous patient monitoring, mitigate risks and maximize therapeutic potential.
Additionally, strict regulatory controls govern the prescription and distribution of cannabis medications to prevent misuse and ensure quality. Standardized formulations, batch testing, and pharmacovigilance programs contribute to maintaining the safety and efficacy of these treatments. Ongoing surveillance systems further refine clinical practices by gathering real-world evidence on patient outcomes and adverse effects.
While significant progress has been made, challenges remain in integrating cannabis into mainstream medicine. Balancing patient access with public safety, advancing research on cannabis components, and increasing education for healthcare providers and patients are essential steps forward. Addressing these challenges will unlock the full potential of cannabis-based therapies, enabling them to address unmet medical needs responsibly and effectively.
By continuing to prioritize safety, ethical considerations, and robust scientific investigation, the medical field can harness the unique properties of cannabis and its components to improve patient outcomes and revolutionize therapeutic approaches for a wide range of conditions.