The Entourage Effect and the Role of Flavonoids
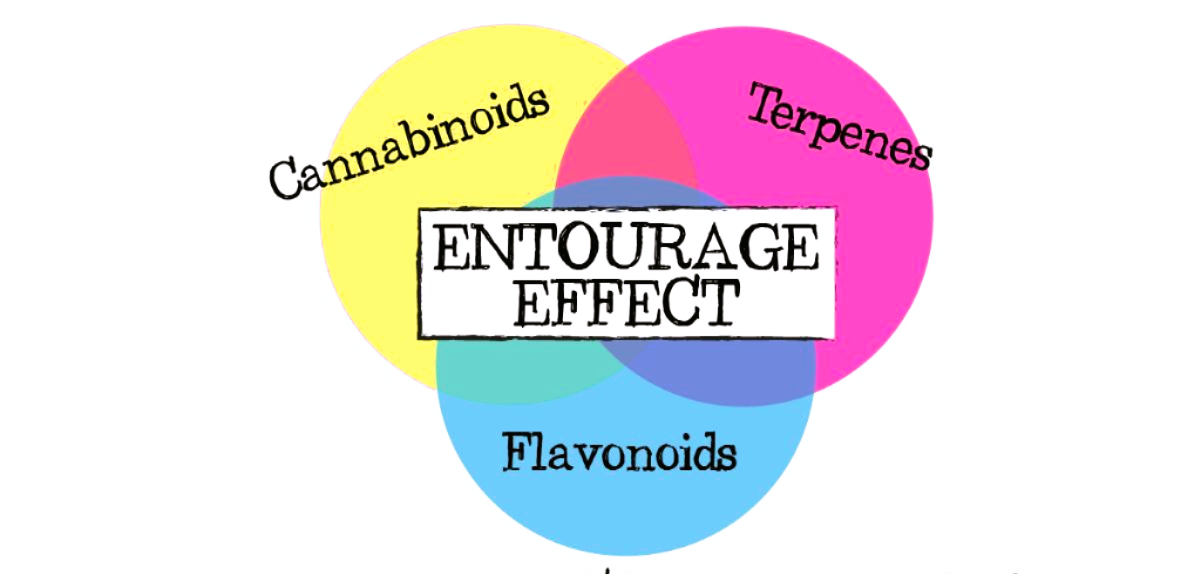
The entourage effect describes how compounds in medicinal plants, especially cannabis, interact to enhance therapeutic benefits. While THC is often highlighted, research now emphasizes the importance of other bioactive compounds, including cannabinoids, terpenes, and flavonoids. Flavonoids, known for their antioxidant and anti-inflammatory properties, are particularly recognized for boosting medicinal effects. This analysis examines the entourage effect from a medical standpoint, focusing on how flavonoids work with other compounds to optimize treatment outcomes across various health conditions.
Understanding Flavonoids and Their Role in Plant Biology
Flavonoids, a class of polyphenolic compounds found abundantly in various plants, serve critical functions in plant biology. These compounds, produced by plants as secondary metabolites, aid in UV filtration, symbiotic nitrogen fixation, and floral pigmentation, attracting pollinators and defending against pathogens. Over 6,000 different flavonoids have been identified across the plant kingdom, and they are divided into several subclasses, including flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, and isoflavonoids. Each subclass possesses unique structural characteristics that impart specific biological activities, contributing to the overall health-promoting effects of the plants that produce them.
In the context of medicinal cannabis, approximately 20 different flavonoids have been identified, including well-known compounds such as apigenin, quercetin, kaempferol, and cannflavins A, B, and C. Cannflavins, in particular, are unique to cannabis and demonstrate potent anti-inflammatory effects that surpass those of aspirin. Flavonoids in cannabis contribute to the plant’s aroma, color, and therapeutic profile, providing antioxidant, anti-inflammatory, and neuroprotective effects. When these flavonoids interact with cannabinoids and terpenes, they are thought to enhance the therapeutic benefits of cannabis through the entourage effect, adding another dimension to the plant’s medicinal potential.
The Synergistic Mechanisms of the Entourage Effect
The entourage effect is not merely a pharmacological curiosity but a paradigm shift in our understanding of plant-based medicine. Traditional pharmacology has often operated on the assumption that isolating and amplifying the active ingredient yields the most effective treatment. However, the entourage effect suggests that the medicinal efficacy of certain compounds can be significantly enhanced when administered in conjunction with others. This effect has been observed across different classes of compounds in cannabis, including cannabinoids, terpenes, and flavonoids, all of which interact with the body’s endocannabinoid system (ECS) and other biochemical pathways.
In terms of medical applications, the entourage effect can lead to a broader therapeutic index, where a combination of compounds may yield desired effects with fewer side effects than a single isolated compound. For instance, while THC alone may cause psychoactive effects that are undesirable in some medical settings, the presence of cannabidiol (CBD) can mitigate these effects while enhancing THC’s therapeutic properties, such as pain relief and anti-inflammation. Similarly, flavonoids contribute their own set of properties, such as enhancing bioavailability and modulating immune responses, which can be pivotal in treating various medical conditions.
The Biological Mechanisms of Flavonoids in Medical Therapy
Flavonoids exert their effects through multiple biological pathways, making them versatile agents in medical therapy. They act as antioxidants by scavenging free radicals, reducing oxidative stress, and preventing cellular damage. Their anti-inflammatory properties are mediated through the inhibition of pro-inflammatory cytokines and enzymes like cyclooxygenase (COX) and lipoxygenase (LOX), which are involved in the inflammatory response. Additionally, flavonoids can modulate gene expression, inhibit cancer cell proliferation, induce apoptosis in malignant cells, and offer neuroprotective benefits by interacting with neuronal receptors.
These biological activities are beneficial in managing a variety of medical conditions. Flavonoids’ antioxidant properties, for instance, can aid in the treatment of neurodegenerative illnesses like Parkinson’s and Alzheimer’s, where oxidative stress is a major factor in the development of the disease. The anti-inflammatory effects are beneficial for chronic inflammatory conditions such as arthritis and inflammatory bowel disease, where reducing inflammation can alleviate pain and improve quality of life. The anticancer properties of certain flavonoids also hold promise for oncology, as they can inhibit cancer cell growth and potentially improve outcomes when used alongside conventional treatments.
Flavonoids in Cannabis: Cannflavins and Their Anti-Inflammatory Potential
Cannflavins, a group of flavonoids unique to cannabis, have garnered significant interest for their powerful anti-inflammatory properties. Cannflavins A, B, and C have been shown to inhibit pro-inflammatory mediators like prostaglandin E2, which is involved in inflammation and pain pathways. Cannflavin A, in particular, has been found to be nearly 30 times more effective than aspirin in inhibiting COX enzymes, which are responsible for pain and inflammation. This has profound implications for pain management, especially in conditions such as arthritis, where inflammation contributes to chronic pain and joint degradation.
For patients seeking alternatives to nonsteroidal anti-inflammatory drugs (NSAIDs), which can have adverse effects on the gastrointestinal tract and cardiovascular system, cannflavins offer a promising, plant-based option. By potentially reducing the need for high-dose NSAIDs or opioids in pain management, cannflavins could lead to a safer treatment regimen with fewer side effects, particularly for patients with chronic inflammatory conditions. Additionally, the anti-inflammatory properties of cannflavins may benefit patients with autoimmune diseases, such as multiple sclerosis, where inflammation and immune dysregulation play a central role in disease progression.
Neuroprotective Properties of Flavonoids in Neurological Disorders
The progressive loss of neuronal structure and function is a hallmark of neurodegenerative illnesses like Parkinson’s and Alzheimer’s. Although the precise processes behind these illnesses are intricate and varied, neuronal damage is known to be caused by oxidative stress and inflammation. Flavonoids, through their antioxidant and anti-inflammatory properties, have shown promise in neuroprotective applications, which could potentially slow disease progression and alleviate symptoms.
Research indicates that certain flavonoids can cross the blood-brain barrier, allowing them to exert direct effects on the central nervous system. For instance, quercetin, a flavonoid found in many plants, has been shown to protect neurons from oxidative damage and may inhibit the formation of beta-amyloid plaques, which are characteristic of Alzheimer’s disease. Apigenin, another flavonoid, has been studied for its anxiolytic and neuroprotective effects, which are thought to result from its interaction with gamma-aminobutyric acid (GABA) receptors in the brain. By modulating these pathways, flavonoids could offer a complementary approach to conventional neuroprotective treatments, potentially reducing the need for pharmaceutical intervention or enhancing the efficacy of existing therapies.
Anti-Cancer Properties of Flavonoids and Their Role in Oncology
The anti-cancer potential of flavonoids has been a subject of extensive research. Flavonoids such as quercetin, kaempferol, and luteolin have demonstrated anticancer properties in preclinical studies, showing the ability to inhibit cancer cell proliferation, induce apoptosis, and suppress angiogenesis—the process by which tumors develop new blood vessels to support their growth. These properties are particularly valuable in oncology, as flavonoids could potentially inhibit tumor growth, enhance the efficacy of chemotherapy, and reduce side effects associated with conventional cancer treatments.
In the context of the entourage effect, the anti-cancer potential of flavonoids may be enhanced when combined with cannabinoids, such as CBD, which has also demonstrated anticancer effects. Research suggests that CBD can inhibit the growth of cancer cells and induce apoptosis, potentially complementing the effects of flavonoids. Together, cannabinoids and flavonoids could provide a multi-targeted approach to cancer treatment, attacking cancer cells through different pathways and reducing the likelihood of resistance. Additionally, by modulating immune function and reducing inflammation, flavonoids may enhance the body’s natural ability to recognize and eliminate cancer cells, contributing to a holistic approach to cancer therapy.
The Role of Flavonoids in Cardiovascular Health
Cardiovascular diseases (CVDs), including hypertension, atherosclerosis, and heart disease, are leading causes of morbidity and mortality worldwide. Oxidative stress and inflammation are critical factors in the development of CVDs, contributing to endothelial dysfunction, plaque formation, and vascular inflammation. Flavonoids, through their antioxidant and anti-inflammatory properties, have shown promise in promoting cardiovascular health and potentially preventing the progression of CVDs.
For instance, flavonoids can improve endothelial function by enhancing nitric oxide availability, which relaxes blood vessels and reduces blood pressure. Quercetin and kaempferol, two flavonoids found in cannabis and other plants, have been shown to lower blood pressure and reduce cholesterol levels, contributing to improved cardiovascular outcomes. By reducing inflammation, flavonoids may also inhibit the development of atherosclerosis, where chronic inflammation leads to plaque buildup in the arteries. In combination with cannabinoids, which also demonstrate cardiovascular benefits, flavonoids could play a role in a multifaceted approach to cardiovascular health, potentially offering a plant-based alternative to conventional treatments.
Immune Modulation and the Potential for Autoimmune Disease Management
Complex and frequently challenging to treat, autoimmune illnesses are defined by an overreaction of the immune system to the body’s own tissues. Conditions such as multiple sclerosis, rheumatoid arthritis, and lupus involve chronic inflammation and immune dysregulation, leading to tissue damage and a range of debilitating symptoms. Flavonoids, with their ability to modulate immune function and reduce inflammation, have shown potential as therapeutic agents in the management of autoimmune diseases.
Research suggests that flavonoids can inhibit the production of pro-inflammatory cytokines, which play a key role in autoimmune pathology. Furthermore, flavonoids may lessen the intensity of autoimmune assaults by restoring immune system homeostasis through the modulation of immune cell activity. In multiple sclerosis, for example, flavonoids may protect neuronal cells from inflammatory damage and potentially slow disease progression. When combined with cannabinoids, which also possess immunomodulatory properties, flavonoids could offer a complementary approach to managing autoimmune diseases, providing relief from symptoms and potentially reducing the need for immunosuppressive drugs.
Flavonoids and Pain Management: A Natural Alternative to Conventional Analgesics
For individuals with chronic pain problems such fibromyalgia, arthritis, and neuropathic pain, pain management is an essential element of medical care. Traditional analgesics, including opioids and NSAIDs, are associated with a range of side effects, including addiction, gastrointestinal damage, and cardiovascular risk. Flavonoids, with their potent anti-inflammatory and analgesic properties, offer a natural alternative for pain management, potentially reducing the need for high-dose analgesics.
As previously mentioned, cannflavins in cannabis have been found to inhibit COX enzymes, which are involved in pain and inflammation pathways. By targeting these enzymes, cannflavins may provide pain relief without the gastrointestinal risks associated with NSAIDs. Additionally, flavonoids like apigenin and quercetin have demonstrated analgesic effects in preclinical studies, suggesting that they could be beneficial in managing chronic pain conditions. When combined with cannabinoids, which also provide pain-relieving effects, flavonoids could enhance the efficacy of cannabis-based treatments for pain management, offering a safer alternative to traditional analgesics.
Restrictions on Using Cannabis in the Medical Field as a Last Resort and Monitoring THC Levels

The medical use of cannabis has gained traction worldwide, offering potential benefits for various health conditions due to its therapeutic compounds. However, medical cannabis remains a subject of rigorous regulation, primarily to minimize psychoactive effects and ensure that it is used judiciously. Restricting cannabis in the medical field as a last-resort treatment underscores the need for prudence and highlights the necessity of monitoring THC levels in medications to protect patients from unintended psychoactive experiences.
Cannabis as a Last Resort in Medical Treatment
One of the central tenets guiding the medical use of cannabis is its role as a last-resort treatment, which is generally reserved for patients who have exhausted traditional medical options. This approach is intended to safeguard patients by ensuring that cannabis is used only when other therapies have proven insufficient or intolerable. For example, in cases of chronic pain, epilepsy, or chemotherapy-induced nausea, patients may not respond well to conventional medications or may suffer from severe side effects. In such instances, cannabis, particularly formulations with non-psychoactive components like cannabidiol (CBD), has shown promise.
Using cannabis as a last resort in medical practice also mitigates risks associated with dependency and side effects, allowing healthcare providers to avoid over-reliance on a single treatment. This measured approach requires a thorough review of a patient’s medical history, previous treatments, and their outcomes. Once these alternatives have been exhausted, cannabis may be introduced as part of a broader therapeutic regimen, often as an adjunct to other treatments, under strict medical supervision.
Monitoring THC Levels to Prevent Psychoactive Effects
A major concern in medical cannabis use is the psychoactive effects associated with tetrahydrocannabinol (THC), one of its primary cannabinoids. High levels of THC can induce altered mental states, including euphoria, anxiety, and hallucinations, which are generally undesirable in a medical context. To prevent these effects, it is essential to monitor and control THC levels in cannabis-based medications. Many countries and medical institutions mandate that THC levels remain below a certain threshold in medicinal formulations, particularly when patients need to remain functional, alert, and free from psychoactive experiences.
Various cannabis strains and extracts contain differing THC concentrations, and selecting or modifying these strains allows for precise dosing. Medical formulations often include higher levels of CBD, which is non-psychoactive and known to counterbalance THC’s effects. The ratio of THC to CBD is carefully adjusted to maximize therapeutic benefits while minimizing psychoactivity. For instance, in treating chronic pain, a low-THC, high-CBD product may provide relief without compromising cognitive function. Regular testing of these formulations is vital, and regulatory bodies often require that THC levels be quantified in lab analyses before medical cannabis products reach patients.
Regulatory Guidelines and Professional Oversight
To ensure responsible use, regulatory agencies worldwide have established guidelines for medical cannabis prescriptions, requiring that healthcare providers receive training on appropriate usage, dosing, and monitoring. Medical professionals need to follow strict guidelines when prescribing cannabis, including setting clear objectives, such as alleviating specific symptoms or improving quality of life. These professionals must monitor patient responses closely, adjusting dosages as needed and remaining vigilant to any signs of adverse reactions, including potential psychoactivity from THC.
In addition, a framework for patient education is essential in guiding individuals through the potential effects and limitations of medical cannabis. Patients should be well-informed about the possibility of psychoactive effects, even at low THC doses, and advised on recognizing and reporting any negative experiences to their healthcare provider. This proactive approach enables better control of patient outcomes and helps in fine-tuning treatments to ensure they are safe, effective, and tailored to individual needs.
Conclusion
In summary, the medical application of cannabis and its components presents a promising yet complex frontier in healthcare. The concept of the entourage effect emphasizes how various compounds within cannabis, including cannabinoids, terpenes, and flavonoids, work synergistically to amplify therapeutic benefits beyond what any single component could achieve alone. This synergy holds immense potential for managing a range of medical conditions—from chronic pain, inflammation, and neurodegenerative diseases to cancer, cardiovascular health, and autoimmune disorders.
Flavonoids, in particular, contribute significantly to this entourage effect, providing potent antioxidant, anti-inflammatory, neuroprotective, and immune-modulating properties that complement and enhance the actions of cannabinoids. Unique flavonoids like cannflavins, with their powerful anti-inflammatory effects, offer promising natural alternatives to conventional medications, particularly for conditions requiring long-term management.
However, integrating cannabis into medical practice requires a responsible approach, positioning it as a last-resort therapy after exhausting conventional options. Restricting medical cannabis use and carefully monitoring THC levels ensure that patients receive therapeutic benefits without unintended psychoactive effects, aligning with the goal of improving quality of life in a safe, controlled manner. Professional oversight, regulatory guidelines, and patient education are essential to maintaining a balance between efficacy and safety, particularly in managing complex medical conditions.
Through a combination of scientific rigor, careful regulation, and personalized care, cannabis can be responsibly harnessed as a powerful medicinal tool, providing relief and enhancing outcomes for patients in need. The therapeutic potential of cannabis lies not only in its individual components but in the harmonious interplay of these compounds, underscoring the importance of holistic, plant-based approaches in advancing medical treatments.