
Supporting Gut Health with Medical Cannabis: The Gut-Brain Axis and IBS
Introduction
The relationship between gut health and overall well-being has gained significant attention in recent years, with growing recognition of the gut-brain axis as a critical factor in various health conditions, particularly those related to gastrointestinal (GI) function. Among these conditions, Irritable Bowel Syndrome (IBS) stands out due to its widespread prevalence and complex symptomatology. While conventional treatments for IBS often focus on symptom management, there is a burgeoning interest in the potential role of medical cannabis in supporting gut health through its interaction with the gut-brain axis. This paper explores the scientific basis of this relationship, the potential benefits of medical cannabis for gut health, and its specific application in the management of IBS.
The Gut-Brain Axis: An Overview
This two-way communication network, known as the gut-brain axis, connects the central nervous system (CNS) and the enteric nervous system (ENS) of the gastrointestinal tract. This connection is facilitated by a complex interplay of neural, hormonal, and immune pathways, which collectively regulate a wide range of physiological processes, including digestion, mood, and immune response.
Components of the Gut-Brain Axis
- The Enteric Nervous System (ENS): Often referred to as the “second brain,” the ENS is a vast network of neurons embedded within the walls of the GI tract. It controls local GI functions such as motility, secretion, and blood flow, largely independent of the CNS, although it remains connected to the brain through the autonomic nervous system.
- The Central Nervous System (CNS): The CNS, comprising the brain and spinal cord, communicates with the gut through both the sympathetic and parasympathetic branches of the autonomic nervous system. This communication is essential for coordinating responses to various stimuli, including stress, food intake, and infection.
- Neurotransmitters and Hormones: Neurotransmitters such as serotonin, dopamine, and acetylcholine, along with hormones like cortisol, play critical roles in the gut-brain axis. For example, approximately 90% of the body’s serotonin is produced in the gut, where it influences GI motility and sensitivity.
- The Microbiome: Trillions of bacteria make up the gut microbiome, which is an important component of the gut-brain axis. These bacteria also interact with the immune system, which further affects gut-brain communication, and they create metabolites that can affect behavior and brain function.
- The Immune System: The immune system, particularly the gut-associated lymphoid tissue (GALT), is intimately involved in maintaining gut health and modulating the gut-brain axis. Inflammatory responses and immune activation within the gut can have far-reaching effects on CNS function and overall health.
Irritable Bowel Syndrome (IBS): A Complex Disorder
IBS is a functional GI disorder characterized by a combination of symptoms including abdominal pain, bloating, and altered bowel habits (diarrhea, constipation, or a mix of both). Despite its prevalence, the exact cause of IBS remains elusive, with a combination of genetic, environmental, and psychological factors thought to contribute to its development.
Pathophysiology of IBS
- Visceral Hypersensitivity: One of the hallmark features of IBS is visceral hypersensitivity, where patients experience heightened pain in response to normal gut stimuli. This increased sensitivity is thought to result from alterations in the gut-brain axis, including changes in neurotransmitter levels and nerve signaling.
- Altered Gut Motility: IBS patients often exhibit abnormal gut motility, leading to symptoms such as diarrhea or constipation. These changes may be related to dysregulation of the ENS, which controls the coordinated contractions of the GI tract.
- Gut Microbiome Dysbiosis: According to new research, IBS may be linked to changes in the gut microbiome, such as an imbalance between good and bad bacteria and a decrease in microbial diversity. These changes can affect gut-brain communication and contribute to symptoms.
- Inflammation and Immune Activation: Low-grade inflammation and immune system activation have been observed in some IBS patients, particularly those with post-infectious IBS. This inflammation can affect gut permeability, leading to increased sensitivity and altered gut function.
- Psychological Factors: Psychological issues such as stress, worry, and depression are frequently linked to IBS and have the potential to worsen its symptoms. The gut-brain axis is a critical mediator of this relationship, with stress affecting gut motility, sensitivity, and immune function.
The Role of Medical Cannabis in Gut Health
Medical cannabis, derived from the Cannabis sativa plant, contains a variety of bioactive compounds, including cannabinoids, terpenes, and flavonoids, which have been shown to interact with the body’s endocannabinoid system (ECS). The ECS is a complex signaling network that plays a key role in maintaining homeostasis across various physiological systems, including the GI tract.
The Endocannabinoid System and Gut Health
The ECS consists of three main components:
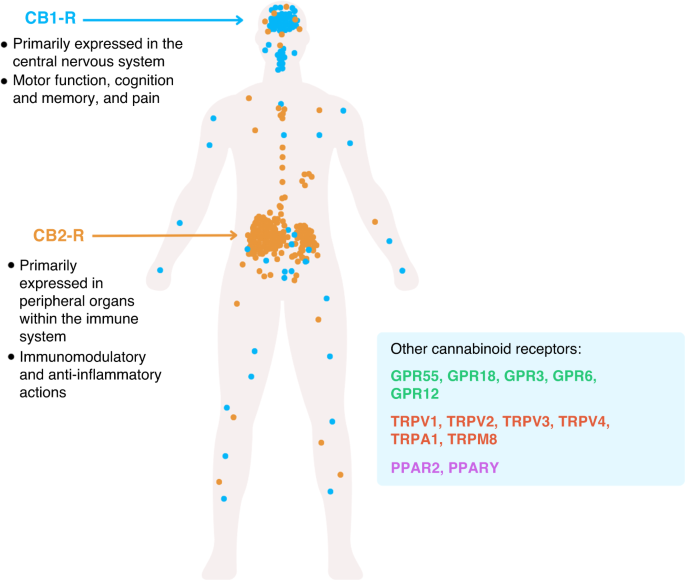
- Cannabinoid Receptors (CB1 and CB2): These receptors are widely distributed throughout the body, including the GI tract and the brain. CB1 receptors are primarily found in the CNS and ENS, where they modulate neurotransmitter release and gut motility. CB2 receptors are mainly located in immune cells, where they regulate inflammation and immune responses.
- Endogenous Cannabinoids (Endocannabinoids): The body produces its own cannabinoids, such as anandamide and 2-arachidonoylglycerol (2-AG), which bind to and activate cannabinoid receptors. These endocannabinoids are involved in regulating various processes, including pain perception, inflammation, and gut motility.
- Enzymes: Endocannabinoids are synthesized and degraded by enzymes including fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL), which regulates the body’s levels and activity of these molecules.
Cannabinoids and Their Effects on the Gut
Phytocannabinoids, the cannabinoids found in the cannabis plant, can mimic the effects of endocannabinoids by interacting with CB1 and CB2 receptors. The two most well-known phytocannabinoids are:
- Tetrahydrocannabinol (THC): The main psychoactive ingredient in cannabis, THC, binds to CB1 receptors with great affinity. In the context of gut health, THC has been shown to reduce gut motility, decrease visceral pain, and modulate immune responses.
- Cannabidiol (CBD): The non-psychoactive cannabis compound CBD is becoming more well-known for its analgesic, anxiolytic, and anti-inflammatory qualities. Unlike THC, CBD has a low affinity for CB1 and CB2 receptors but can modulate the ECS indirectly by inhibiting the degradation of endocannabinoids and interacting with other receptor systems.
Other lesser-known cannabinoids, such as cannabigerol (CBG) and cannabichromene (CBC), also exhibit potential therapeutic effects on gut health through their interaction with the ECS.
Mechanisms of Action
- Modulation of Gut Motility: Cannabinoids can influence gut motility through their effects on CB1 receptors in the ENS. THC, in particular, has been shown to reduce hypermotility, which may help alleviate diarrhea-predominant IBS. Conversely, the activation of CB2 receptors can reduce inflammation-related changes in gut motility, which may benefit patients with constipation-predominant IBS.
- Reduction of Visceral Pain: Visceral hypersensitivity is a major contributor to the pain experienced by IBS patients. Cannabinoids can reduce this pain by modulating the release of neurotransmitters and decreasing the activation of pain pathways in the CNS and ENS. In animal models of visceral pain, THC and CBD have both been demonstrated to have analgesic benefits.
- Anti-Inflammatory Effects: Inflammation plays a role in the pathophysiology of IBS, particularly in post-infectious cases. Cannabinoids, particularly CBD, have potent anti-inflammatory properties, mediated through the activation of CB2 receptors and other pathways. These anti-inflammatory effects may help reduce gut inflammation and improve symptoms in IBS patients.
- Modulation of the Gut Microbiome: The gut microbiome plays a critical role in gut health and the gut-brain axis. The composition and activity of the gut microbiome may be influenced by cannabis, however research in this field is still in its infancy. For example, studies have shown that cannabis use is associated with changes in microbial diversity and an increase in beneficial bacteria.
- Anxiolytic and Antidepressant Effects: Given the strong association between psychological factors and IBS, the anxiolytic and antidepressant effects of cannabinoids, particularly CBD, may also contribute to their therapeutic potential. By reducing stress and anxiety, cannabinoids may help alleviate the psychological triggers that exacerbate IBS symptoms.
Medical Cannabis and IBS: Clinical Evidence
While the potential mechanisms of action of cannabinoids in gut health are well-supported by preclinical studies, clinical evidence for the use of medical cannabis in IBS remains limited but promising.
Clinical Trials and Studies
- Pain Relief and Gut Motility: A double-blind, placebo-controlled trial conducted in the UK investigated the effects of THC on gut motility and visceral pain in IBS patients. The study found that THC significantly reduced pain and decreased colonic motility in patients with diarrhea-predominant IBS. These findings suggest that THC may be particularly beneficial for patients with IBS-D.
- Anti-Inflammatory Effects: Another study evaluated the effects of CBD on inflammation and gut permeability in patients with post-infectious IBS. The results showed that CBD reduced markers of inflammation and improved gut barrier function, suggesting a potential role for CBD in managing inflammation-related IBS symptoms.
- Psychological Symptoms: A study conducted in Italy explored the effects of a CBD-rich cannabis extract on anxiety and depression in IBS patients. The study found significant improvements in both anxiety and depression scores, which were associated with a reduction in IBS symptoms. These results demonstrate how CBD may be useful in treating the psychosocial components of IBS.
- Gut Microbiome: Preliminary research has also explored the impact of cannabinoids on the gut microbiome in IBS patients. A study published in the journal Gut Microbes reported that cannabis use was associated with an increase in microbial diversity and a shift towards a more balanced microbiome composition in IBS patients. While these findings are encouraging, further research is needed to confirm the long-term effects of cannabis on the gut microbiome.
Case Reports and Patient Experiences
In addition to clinical trials, numerous case reports and patient testimonials have documented the benefits of medical cannabis for IBS. Cannabis use has been associated with notable improvements in pain, bloating, and bowel movements in patients, frequently following the failure of traditional treatments to produce relief. Although they don’t replace scientific proof, these anecdotal tales offer insightful information about the practical uses of medicinal cannabis in the treatment of IBS.
Safety and Considerations for Medical Use
While the potential benefits of medical cannabis for gut health and IBS are significant, it is important to consider the safety and appropriate use of this therapy, particularly in the context of long-term treatment.
Safety Profile of Cannabinoids
- THC: While THC has demonstrated efficacy in reducing pain and modulating gut motility, its psychoactive effects limit its use, particularly in patients who may be sensitive to these effects. Long-term use of THC is also associated with potential risks such as cognitive impairment, dependence, and tolerance. As a result, THC is often used at lower doses or in combination with CBD to mitigate these risks.
- CBD: CBD has a more favorable safety profile compared to THC, with minimal psychoactive effects and a lower risk of dependence. However, high doses of CBD can cause side effects such as fatigue, diarrhea, and changes in appetite. Because CBD can alter the metabolism of some drugs, it’s also necessary to take into account any drug interactions.
- Drug Interactions: THC and CBD have the potential to interact with other drugs, especially those that are processed by the CYP450 liver enzymes. This interaction can affect the efficacy and safety of concomitant medications, so it is important for patients to consult with their healthcare provider before starting cannabis therapy.
- Contraindications: Medical cannabis may not be suitable for all patients, particularly those with a history of substance abuse, certain psychiatric conditions, or severe cardiovascular disease. A thorough assessment by a healthcare provider is essential to determine the appropriateness of cannabis therapy for individual patients.
Legal and Regulatory Considerations
The legal status of medical marijuana varies greatly between states and regions; while some strictly forbid its use, others permit it for certain medical ailments. In order to maintain compliance with local rules, patients and healthcare professionals need to negotiate diverse legal environments. Additionally, the lack of standardized dosing and quality control in cannabis products presents challenges in ensuring consistent and safe treatment.
Future Directions and Research
The use of medical cannabis for gut health and IBS is a rapidly evolving field, with ongoing research exploring the full extent of its therapeutic potential. Several key areas warrant further investigation:
- Long-Term Safety and Efficacy: While short-term studies have shown promising results, there is a need for long-term studies to evaluate the safety and efficacy of medical cannabis in IBS patients over extended periods. These studies should also explore the potential development of tolerance and dependence with long-term use.
- Cannabinoid Profiles: Future research should explore the effects of different cannabinoid profiles on gut health and IBS. For example, the role of minor cannabinoids such as CBG and CBC, as well as the potential synergistic effects of whole-plant extracts, should be investigated.
- Personalized Medicine: Optimizing the use of medicinal cannabis in the management of IBS may be possible through the development of tailored therapeutic approaches based on unique patient features, such as genetic variables, microbiome makeup, and ECS function.
- Mechanistic Studies: While the basic mechanisms of action of cannabinoids on the gut-brain axis are understood, further research is needed to elucidate the precise molecular pathways involved. This knowledge could lead to the development of targeted therapies that maximize the benefits of cannabis while minimizing potential side effects.
- Regulatory Frameworks: As the medical use of cannabis continues to expand, there is a need for standardized regulatory frameworks that ensure the quality, safety, and consistency of cannabis products. This includes the development of guidelines for dosing, product labeling, and patient monitoring.
Restrictions on Using Cannabis in Medical Cases as a Last Resort
When considering the use of cannabis in medical cases, particularly as a last resort, several important restrictions and considerations must be addressed to ensure patient safety and the ethical application of this treatment. These restrictions are crucial, especially in sensitive cases like the management of Irritable Bowel Syndrome (IBS) and other conditions where conventional treatments may have failed or provided limited relief.
1. Legal and Regulatory Restrictions
The legal status of medical cannabis varies widely across jurisdictions, and in many places, its use is highly regulated or restricted. In some regions, cannabis may only be prescribed when all other conventional treatments have proven ineffective, a concept known as the “last resort” principle. This principle often comes with specific conditions:
- Approval Process: In jurisdictions where medical cannabis is considered a last resort, the approval process may require multiple layers of authorization, including endorsements from specialists, the submission of detailed patient histories, and evidence that all other treatment options have been exhausted.
- Specific Indications: Cannabis may be approved only for specific medical conditions recognized by regulatory bodies, such as chronic pain, epilepsy, or multiple sclerosis. For IBS and other functional GI disorders, the use of cannabis might require additional justification, particularly if the condition is not listed as an approved indication.
- Patient Consent: Informed consent is critical when considering cannabis as a last-resort treatment. Patients must be fully informed of the potential risks, benefits, and uncertainties associated with cannabis use, especially given the psychoactive effects of THC.
2. Clinical Guidelines and Protocols
In medical practice, the use of cannabis as a last resort should be guided by stringent clinical protocols designed to ensure that it is used safely and effectively:
- Comprehensive Assessment: Before considering cannabis, a thorough assessment of the patient’s medical history, current treatments, and overall health status should be conducted. This assessment should include a review of all previously tried therapies and the reasons for their failure.
- Multidisciplinary Approach: Decisions about using cannabis as a last resort should involve a multidisciplinary team, including gastroenterologists, pain specialists, psychiatrists, and pharmacists. This collaborative approach ensures that all potential treatment options are considered and that cannabis is only used when absolutely necessary.
- Risk-Benefit Analysis: A detailed risk-benefit analysis should be performed, weighing the potential benefits of cannabis against the risks, particularly the psychoactive effects of THC and the potential for dependency or other adverse effects. This analysis has to be routinely checked and documented.
- Monitoring and Follow-Up: It is crucial to keep a close eye on how the patient is responding to cannabis. This entails routine follow-up appointments to evaluate the efficacy of the therapy, identify any side effects, and determine whether continued therapy is necessary. These assessments should serve as the basis for treatment plan modifications.
3. Monitoring THC Levels to Prevent Psychoactive Effects
One of the primary concerns with the use of cannabis in medical cases is the psychoactive effect of THC (tetrahydrocannabinol). While THC has therapeutic properties, its psychoactive effects can pose risks, particularly for patients who may be sensitive to these effects or those who need to maintain cognitive function and daily responsibilities.
Strategies for Monitoring and Controlling THC Levels
- Dose Limitation: The most straightforward approach to minimizing psychoactive effects is to limit the dose of THC administered. Low doses of THC can provide therapeutic benefits, such as pain relief, without significant psychoactive effects. Dosing should be carefully titrated, starting with the lowest effective dose and adjusting as necessary.
- Use of CBD-Rich Strains: CBD (cannabidiol) is a non-psychoactive cannabinoid that can counteract some of the psychoactive effects of THC. By using cannabis strains or products that are rich in CBD and low in THC, the psychoactive impact can be reduced while still providing therapeutic benefits. Some formulations are specifically designed to have high CBD and low THC ratios for this purpose.
- Pharmacological Monitoring: In some cases, it may be necessary to monitor THC levels pharmacologically, using blood tests or other biomarkers to ensure that THC concentrations remain within a safe range. This is particularly important in patients who may be at risk for adverse reactions or who require precise control over THC exposure.
- Formulation and Administration: The method of cannabis administration can also influence the psychoactive effects. Formulations that release THC slowly, such as those designed for extended-release, may reduce the intensity of psychoactive effects. Additionally, some products are engineered to minimize the absorption of THC into the bloodstream, thereby reducing its psychoactive impact.
- Patient Education: Educating patients about the potential psychoactive effects of THC is crucial. Patients should be aware of the signs of intoxication, such as dizziness, altered perception, or impaired judgment, and should be instructed to avoid activities that require full cognitive function, such as driving, during treatment.
Special Considerations for Vulnerable Populations
- Pediatric and Adolescent Patients: In young patients, the use of cannabis, particularly THC, is highly controversial due to concerns about its impact on brain development. If cannabis is considered as a last resort in these populations, extreme caution must be exercised, with strict limitations on THC exposure and close monitoring for any signs of cognitive or behavioral changes.
- Elderly Patients: Elderly patients may be more susceptible to the psychoactive effects of THC, as well as to other potential side effects such as dizziness and confusion. Lower doses of THC and higher proportions of CBD are often recommended for these patients, along with regular monitoring to assess tolerability and effectiveness.
- Patients with Mental Health Conditions: Individuals with a history of mental health disorders, particularly those prone to anxiety, depression, or psychosis, may be at increased risk of adverse effects from THC. In such cases, the use of THC should be carefully considered, and CBD-dominant products should be prioritized to minimize the risk of exacerbating psychiatric symptoms.
4. Ethical Considerations and Patient Rights
The use of cannabis as a last resort raises several ethical considerations, particularly regarding patient autonomy, informed consent, and the right to access potentially beneficial treatments:
- Patient Autonomy: Patients should have the right to make informed decisions about their treatment, including the use of cannabis as a last resort. Healthcare professionals must ensure that patients are properly informed about the potential hazards and advantages of cannabis therapy while also respecting their right to autonomy.
- Informed Consent: Informed consent is not just a legal requirement but an ethical imperative. Patients must be provided with all relevant information about the potential psychoactive effects of THC, the limitations of cannabis as a treatment, and alternative options. To help patients make wise decisions, this information should be provided in an easy-to-understand style.
- Access and Equity: Access to medical cannabis should be equitable, ensuring that all patients who may benefit from this therapy have the opportunity to consider it as an option. This includes addressing potential barriers such as cost, availability, and legal restrictions that may disproportionately affect certain populations.
Conclusion
The interaction between the gut-brain axis and the endocannabinoid system offers a compelling framework for understanding the potential role of medical cannabis in supporting gut health and managing IBS. While current evidence supports the therapeutic benefits of cannabinoids in reducing pain, modulating gut motility, and addressing inflammation, further research is needed to fully elucidate their role in IBS treatment. As the field continues to evolve, medical cannabis may emerge as a valuable adjunct to conventional therapies, offering hope to patients struggling with this challenging condition.
In the meantime, patients and healthcare providers must work together to navigate the complexities of cannabis therapy, ensuring its safe and effective use within the context of evidence-based medicine. By continuing to explore the potential of medical cannabis, we may unlock new avenues for improving gut health and enhancing the quality of life for those affected by IBS.