Table of Contents
Is marijuana a blood thinner
Marijuana, also known as cannabis, has been widely studied for its diverse physiological effects, especially as its medical use becomes increasingly accepted. One of the questions frequently raised is whether marijuana acts as a blood thinner. Understanding this is important, particularly for individuals who are already on anticoagulant therapy or those with clotting disorders.
Understanding Blood Thinners
Blood thinners fall into two main categories:
- Anticoagulants – Medications such as warfarin, heparin, and DOACs (Direct Oral Anticoagulants) that inhibit clotting factors to prevent thrombus formation.
- Antiplatelet Agents – Such as aspirin and clopidogrel, which reduce platelet aggregation.
These drugs are commonly prescribed to patients with atrial fibrillation, deep vein thrombosis, pulmonary embolism, or after cardiovascular interventions.
When people ask if marijuana is a “blood thinner,” they often mean whether it interferes with clot formation or mimics effects of the above drugs.
The Cannabinoid System and Hemostasis
The human endocannabinoid system (ECS) plays a significant role in maintaining homeostasis. Cannabinoids such as THC (delta-9-tetrahydrocannabinol) and CBD (cannabidiol) interact with CB1 and CB2 receptors found throughout the body, including in platelets and the vascular endothelium. Here’s how cannabis could influence blood clotting:

- Platelet Function: Platelets express cannabinoid receptors. In vitro studies show that THC and CBD can influence platelet aggregation.
- Vascular Effects: Cannabinoids have vasodilatory effects that may increase blood flow and indirectly reduce the risk of clot formation.
- Inflammatory Modulation: Cannabis has anti-inflammatory properties, potentially reducing the inflammatory cascade involved in clot development.
Scientific Evidence on Marijuana’s Effect on Blood Clotting
1. Platelet Aggregation
Laboratory studies suggest that THC and CBD can inhibit platelet aggregation under certain conditions. This action mimics antiplatelet medications to some degree, although not as strongly or consistently.
- In vitro research: Studies using platelet-rich plasma indicate that high concentrations of cannabinoids can reduce platelet aggregation, but the effects are variable depending on the presence of other mediators like thrombin or collagen.
- Mechanism: This may occur via inhibition of COX-1 (similar to aspirin), increased cAMP in platelets, or modulation of intracellular calcium levels.
However, these effects are generally weak and not seen at typical recreational doses.
2. Endothelial Effects and Vasodilation
THC is known to cause vasodilation by activating endothelial nitric oxide synthase (eNOS). This can lower blood pressure and increase peripheral circulation. Enhanced blood flow reduces blood viscosity, theoretically reducing the chance of thrombosis.
- A 2010 study published in Cardiovascular Toxicology showed that cannabinoids induced relaxation of vascular smooth muscle, particularly in the mesenteric arteries.
- However, the systemic anticoagulant implications of this are not well-established.
3. Interaction with Coagulation Pathways
There is minimal evidence to suggest that cannabis directly inhibits or enhances coagulation cascade proteins like fibrinogen, thrombin, or Factor Xa. Thus, cannabis is not considered a true anticoagulant.
However, some animal studies show prolonged bleeding time after cannabinoid administration, possibly due to decreased platelet function rather than coagulation cascade interference.
Drug Interactions: Cannabis and Prescription Blood Thinners
One of the most clinically relevant concerns is cannabis interaction with common blood thinners, especially warfarin and DOACs (e.g., apixaban, rivaroxaban).
Warfarin (Coumadin)
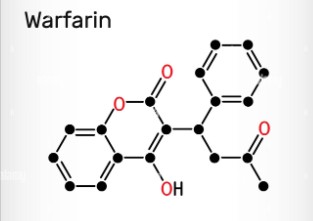
- Warfarin is metabolized by the CYP450 enzyme family, especially CYP2C9.
- THC and CBD both inhibit CYP2C9, potentially increasing warfarin levels in the bloodstream.
- Case reports document increased INR (a measure of blood thinning) in patients using cannabis alongside warfarin, resulting in risk of hemorrhage.
- Recommendation: Patients using warfarin should monitor INR levels closely if consuming cannabis.
Direct Oral Anticoagulants (DOACs)
- These drugs rely less on hepatic metabolism than warfarin but still involve some CYP and P-glycoprotein interactions.
- CBD especially inhibits CYP3A4 and P-gp, which may affect the bioavailability of certain DOACs like rivaroxaban and apixaban.
- Risk level: Moderate – requires physician monitoring.
Cannabidiol (CBD) as a Potential Blood-Thinning Agent
CBD is non-psychoactive but pharmacologically active. In addition to enzyme inhibition, CBD may influence platelet function and systemic inflammation:
- A 2020 animal study in Phytotherapy Research noted that CBD reduced infarct size in rats with induced ischemic stroke, partially due to decreased platelet adhesion and improved blood flow.
- CBD also modulates serotonin and adenosine pathways, which are involved in platelet aggregation and vascular tone.
However, human clinical data is lacking to define CBD as a consistent or safe anticoagulant.
Risk of Bleeding with Marijuana
Cannabis is not typically associated with bleeding risk in healthy individuals. However, combining marijuana with anticoagulants or antiplatelets raises the risk of:
- Nosebleeds
- Easy bruising
- Gastrointestinal bleeding
- Hematuria (blood in urine)
- Prolonged bleeding after injury
These effects may be more prominent in elderly patients, those with liver dysfunction, or individuals on multiple medications.
Clinical Case Reports
Several case studies have highlighted relevant risks:
- Warfarin + Cannabis: A patient using CBD oil while on warfarin showed a dramatic INR rise from 2.5 to 6.5, indicating a significant interaction requiring warfarin dose adjustment.
- Spontaneous Hematomas: Rare cases of deep tissue bleeding in chronic cannabis users have been reported, especially when combined with NSAIDs or anticoagulants.
However, these are rare and usually involve high or chronic cannabis intake with overlapping drug regimens.
Special Considerations
Surgery
Cannabis use may prolong bleeding time during or after surgery, especially in those consuming it daily. Some anesthesiologists recommend stopping cannabis use at least 72 hours before surgery.
Pregnancy
There’s no solid evidence that cannabis affects clotting during pregnancy, but its use is generally discouraged due to fetal development concerns.
Medical Cannabis Patients
Patients using medical marijuana for conditions like chronic pain, multiple sclerosis, or epilepsy who also take blood thinners must inform their physicians to allow safe co-management and INR monitoring.
Summary: Is Marijuana a Blood Thinner?
| Criteria | Effect |
|---|---|
| Antiplatelet-like Action | Mild and inconsistent |
| Anticoagulant Action | Minimal to none |
| Vasodilation | Yes – may promote blood flow |
| Interaction with Warfarin | High – CYP inhibition raises INR |
| Risk of Bleeding (alone) | Low in healthy individuals |
| Risk with Other Drugs | Moderate to high depending on dosage and drug |
Conclusion: Marijuana is not a true blood thinner in the medical sense. However, it has mild antiplatelet-like properties and can interact significantly with prescribed anticoagulants, especially warfarin and possibly DOACs. These interactions are largely due to cannabinoid-induced inhibition of liver enzymes (mainly CYP2C9 and CYP3A4), which can lead to elevated drug levels and increased bleeding risk. While the effects are not uniform across all users, caution is strongly advised for individuals on blood-thinning therapy, and professional medical supervision is essential.