Flavonoids and Pain Management in Medical Cannabis
Flavonoids are bioactive compounds found abundantly in plants and are recognized for their broad therapeutic potential. Within the context of medical cannabis, flavonoids have emerged as significant components due to their potential roles in pain management. This paper delves into the interplay between flavonoids in cannabis and their therapeutic effects in managing pain, with a focus on the biochemical, pharmacological, and clinical implications, strictly for medical use. Although cannabinoids like THC (tetrahydrocannabinol) and CBD (cannabidiol) have received a lot of attention, flavonoids are also becoming recognized for their complimentary and maybe synergistic roles in cannabis, which could increase the plant’s effectiveness in treating pain.
Biochemistry of Flavonoids in Cannabis
Flavonoids are polyphenolic compounds naturally occurring in various fruits, vegetables, and medicinal plants, including cannabis. They belong to a diverse group that includes several subclasses, such as flavones, flavonols, flavanones, flavanonols, and isoflavonoids, each characterized by slight variations in chemical structure but shared bioactive properties. In cannabis, flavonoids constitute about 10% of the bioactive content, with compounds such as cannflavin A, cannflavin B, and cannflavin C being unique to the cannabis plant. These cannabis-specific flavonoids exhibit potent anti-inflammatory and analgesic properties, positioning them as prime candidates in pain management.
Cannflavins A and B, for instance, have been observed to exhibit 30 times the anti-inflammatory potency of aspirin in preclinical studies, acting through pathways independent of the cyclooxygenase (COX) enzymes typically targeted by non-steroidal anti-inflammatory drugs (NSAIDs). These flavonoids work primarily by inhibiting the production of pro-inflammatory mediators, including prostaglandins, which are heavily implicated in the inflammatory response and pain perception. Cannflavins accomplish this by suppressing the biosynthesis of prostaglandins at the cellular level and blocking the release of arachidonic acid, a precursor in prostaglandin synthesis.
Beyond their anti-inflammatory effects, flavonoids interact with various pain-related biochemical pathways. They modulate receptor activity, particularly by interacting with opioid and cannabinoid receptors, which are central to pain perception and regulation. This modulatory ability suggests that flavonoids may potentiate the effects of other cannabis-derived compounds, such as cannabinoids, through an “entourage effect.” The entourage effect theory posits that the therapeutic effects of cannabis are enhanced when cannabinoids, flavonoids, and terpenes work synergistically rather than in isolation, promoting a more comprehensive pain relief profile.
Pharmacodynamics and Pharmacokinetics of Flavonoids
The pharmacodynamics of flavonoids in cannabis in relation to pain relief encompasses their interaction with multiple receptors and enzymes. Cannflavin A and B, as well as other flavonoids like quercetin and apigenin found in cannabis, exhibit selective activity on pain-related pathways without affecting central nervous system pathways that can cause psychoactive side effects. These compounds modulate transient receptor potential (TRP) channels, especially TRPV1 and TRPA1, which are integral to pain and inflammation pathways. By desensitizing these receptors, flavonoids can mitigate hyperalgesia and allodynia, two symptoms associated with chronic pain conditions.
Flavonoids also exhibit pharmacokinetic properties that are conducive to sustained therapeutic effects. They have moderate bioavailability due to their polyphenolic structure, which enables them to remain in circulation longer than more rapidly metabolized compounds. However, challenges remain, as the absorption of flavonoids is often limited by their hydrophilicity. Emerging studies are exploring nanocarriers and other drug-delivery methods to improve flavonoid bioavailability, thereby enhancing their therapeutic potential in medical cannabis products for pain relief.
One important aspect of flavonoids’ pharmacokinetics is their metabolic stability. While they undergo rapid metabolism in the liver, they are also conjugated into various metabolites that retain activity, enabling a prolonged anti-inflammatory and analgesic effect. This extended duration is beneficial in managing chronic pain, where continuous symptom relief is needed.
Clinical Evidence Supporting Flavonoids in Pain Management
Flavonoids have shown promise in the clinical context of pain management, particularly for patients with chronic pain, inflammatory pain, and neuropathic pain. Preclinical trials highlight flavonoids’ analgesic effects in animal models of inflammation and neuropathy. For example, studies on rats demonstrated that cannflavin A reduced inflammatory pain, providing an analgesic effect comparable to pharmaceutical-grade NSAIDs without gastrointestinal side effects commonly associated with these drugs. The suppression of inflammatory cytokines including TNF-α, IL-1β, and IL-6, which all contribute to pain hypersensitivity, is one of the reasons behind these effects.
Clinical trials on human subjects are still limited, but initial findings suggest that flavonoids may play a substantial role in managing conditions like fibromyalgia, arthritis, and other chronic pain disorders. Patients who consume cannabis strains high in flavonoid content report improved pain scores and a better quality of life, particularly in comparison to conventional pain medications. This may be attributed to flavonoids’ multi-targeted approach, providing anti-inflammatory, antioxidant, and analgesic effects concurrently, which is advantageous in managing complex, multifactorial conditions like chronic pain.
In fibromyalgia, a condition characterized by widespread musculoskeletal pain and heightened pain sensitivity, flavonoids may reduce pain severity by modulating inflammatory pathways and enhancing endocannabinoid system function. These mechanisms are also relevant in arthritis, where inflammation plays a prominent role in joint pain and degeneration. In conditions like neuropathy, where pain is often refractory to traditional treatments, the TRPV1 desensitization by flavonoids shows particular promise. While traditional therapies for neuropathic pain, such as antidepressants and anticonvulsants, come with side effects and variable efficacy, flavonoid-rich cannabis offers an alternative with fewer adverse effects and sustained relief.
Anti-inflammatory and Antioxidant Effects in Pain Management
Pain, especially chronic pain, is often intricately linked to inflammation and oxidative stress, both of which contribute to the persistence and exacerbation of pain symptoms. Flavonoids in cannabis offer substantial anti-inflammatory and antioxidant effects, which are integral to pain relief. By scavenging free radicals and reducing oxidative stress, flavonoids prevent the damage of cellular structures and protect against the upregulation of inflammatory mediators. Quercetin, a flavonoid commonly found in cannabis, has demonstrated robust antioxidant properties, protecting cells from oxidative damage, which is prevalent in chronic pain conditions.
Additionally, flavonoids modulate inflammatory pathways by inhibiting nuclear factor kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) pathways. NF-κB is a critical regulator of inflammation, influencing the expression of cytokines, chemokines, and adhesion molecules, all of which contribute to inflammation and pain. By inhibiting these pathways, flavonoids can reduce the activation of immune cells that contribute to pain, effectively mitigating the inflammatory component of chronic pain disorders.
In arthritis, for instance, the reduction of pro-inflammatory markers like IL-1 and TNF-α through flavonoid-rich cannabis formulations can alleviate joint inflammation and pain, providing a non-opioid alternative for long-term pain management. Patients with osteoarthritis and rheumatoid arthritis are frequently affected by inflammation-driven pain and have reported substantial improvements when using cannabis rich in flavonoids and cannabinoids. This suggests a dual-modality approach where flavonoids work alongside cannabinoids to address pain from multiple biochemical angles.
Flavonoids, Cannabinoids, and the Entourage Effect
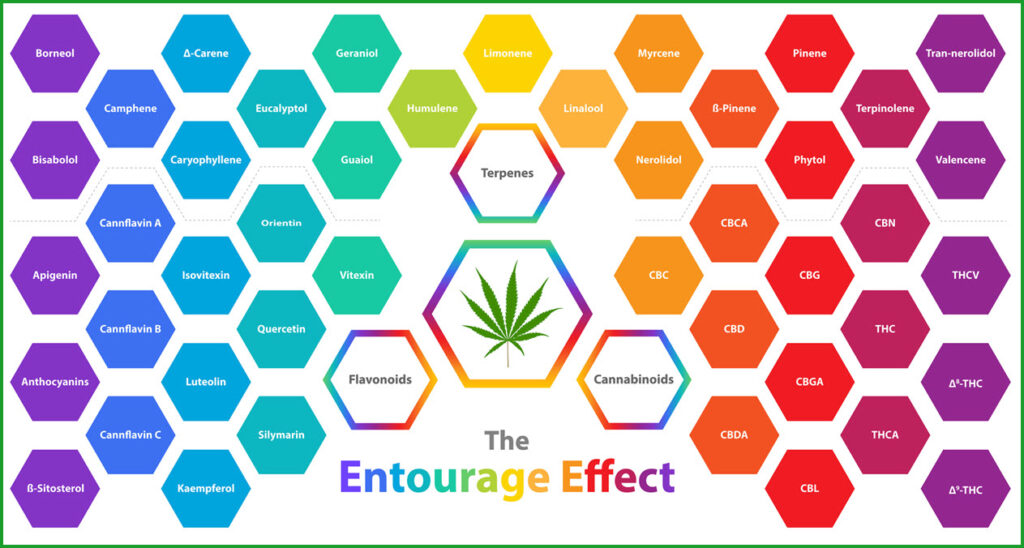
One of the unique aspects of flavonoids in cannabis is their interaction with cannabinoids to create a combined, enhanced therapeutic effect known as the entourage effect. This theory posits that the pharmacological effects of cannabis are optimized when cannabinoids, flavonoids, and terpenes are present in concert, rather than isolated. In the case of pain management, this synergy is particularly evident. Cannabinoids such as THC and CBD interact with CB1 and CB2 receptors in the endocannabinoid system to regulate pain perception and inflammation, while flavonoids enhance these effects through independent but complementary mechanisms.
Research has shown that flavonoids can amplify the analgesic and anti-inflammatory effects of cannabinoids. For instance, quercetin and apigenin, both found in cannabis, may inhibit enzymes that break down endocannabinoids like anandamide, thereby prolonging their analgesic effects. Additionally, flavonoids like cannflavins reduce inflammatory mediators and enhance cannabinoid activity at pain-related receptors, leading to a more potent and longer-lasting analgesic effect.
The entourage effect highlights the importance of whole-plant cannabis extracts in medical applications, as these extracts preserve the natural ratios of cannabinoids, flavonoids, and terpenes. While isolated cannabinoids have demonstrated efficacy in pain management, the inclusion of flavonoids potentially reduces the required dose of cannabinoids, lowering the risk of tolerance and side effects. For patients with chronic pain conditions requiring long-term treatment, this approach can offer effective pain relief with a reduced side effect profile.
Potential and Limitations of Flavonoid Research in Pain Management
While the therapeutic potential of flavonoids in cannabis for pain management is promising, several limitations exist in the current body of research. Clinical trials specifically focused on flavonoids are sparse, with most data derived from animal studies and observational reports. There is also a lack of standardization in flavonoid content across cannabis strains, making it challenging to draw precise correlations between specific flavonoids and therapeutic outcomes.
Moreover, flavonoids in cannabis have complex pharmacokinetic profiles, which may influence their bioavailability and efficacy in pain relief. Given their hydrophilic nature, flavonoids face challenges in absorption and rapid metabolism, which can limit their efficacy in systemic pain management. Advances in delivery methods, such as nanoemulsions and encapsulation, are being explored to overcome these limitations and enhance flavonoid bioavailability.
To clarify the precise processes by which flavonoids alleviate pain and to further investigate their interactions with cannabinoids, more research is necessary. The development of standardized cannabis formulations with consistent flavonoid profiles could enable more reliable and reproducible therapeutic outcomes, ultimately advancing the role of flavonoids in clinical pain management.
Restrictions on Using Cannabis Flavonoids in the Medical Field and Ensuring THC Monitoring as a Last Resort for Pain Management
The use of cannabis components, including flavonoids, in medical treatment, particularly for chronic pain, is gaining interest. However, strict regulatory and ethical guidelines ensure patient safety, recommending cannabis-based products only when conventional therapies are ineffective. Known for their anti-inflammatory and analgesic effects, cannabis flavonoids are restricted to last-resort cases, with careful monitoring of THC levels to prevent psychoactive effects that could impair patient functionality. This approach ensures a safe, non-psychoactive therapeutic option for patients.
Regulatory Restrictions on Cannabis Flavonoids in Medical Treatment
In many regions, the medical use of cannabis and its derivatives is subject to strict regulations, particularly where psychoactive compounds such as THC are concerned. For cannabis flavonoids, although they do not induce psychoactive effects, regulatory bodies often impose restrictions similar to those for cannabinoids to prevent potential misuse or unanticipated interactions with other cannabis components, especially in formulations that include both flavonoids and cannabinoids. These restrictions emphasize that cannabis-based treatments should only be pursued after standard therapeutic options, including NSAIDs, opioids, and non-cannabis-derived anti-inflammatory agents, have proven ineffective or unsuitable due to patient intolerance or contraindications.
Cannabis-based products, including those high in flavonoids, are categorized as controlled substances in many countries, requiring physician authorization and, in some cases, special licensing. Medical professionals must navigate a regulatory landscape that prioritizes the use of conventional treatments and mandates exhaustive documentation to justify the use of cannabis flavonoids as a last-line option. Patients and healthcare providers must demonstrate that other therapies failed or that side effects were prohibitive. This rigorous process helps to limit cannabis use to cases where it is truly medically necessary, ensuring it is not overprescribed or used casually in clinical settings.
Cannabis Flavonoids as a Last-Resort Therapy for Pain Management
The application of cannabis flavonoids as a therapeutic option in pain management is typically recommended only when traditional treatments do not yield satisfactory results. Because chronic pain is complex, finding adequate pain management without unwarranted side effects frequently requires a trial-and-error method. Given the potential benefits of flavonoids in reducing inflammation and alleviating pain, they provide a promising alternative for patients with refractory conditions. However, to ensure safety and efficacy, guidelines encourage clinicians to exhaust other options before considering cannabis-derived therapies.
Flavonoids such as cannflavin A and B, which are unique to cannabis, have shown potent anti-inflammatory effects in preliminary studies, potentially outperforming conventional NSAIDs without associated gastrointestinal side effects. For patients suffering from chronic inflammatory conditions, including arthritis or fibromyalgia, cannabis flavonoids may offer targeted relief when other treatments fail to mitigate pain effectively. However, due to the limited clinical research on flavonoids alone, medical cannabis formulations are often viewed as a last-resort option, ensuring patients have access to a broader array of established therapies first.
Monitoring THC Levels to Avoid Psychoactive Effects
One of the primary concerns with cannabis-derived treatments, even those focused on non-psychoactive components like flavonoids, is the potential presence of THC, the main psychoactive compound in cannabis. For cannabis to be safely incorporated into medical practice, it is essential that THC levels in therapeutic formulations be strictly controlled to prevent psychoactive side effects that could impair a patient’s cognitive or motor functions. Regulatory authorities in many countries have established stringent THC limits for medical cannabis products, often setting thresholds below 0.3% or even lower for therapeutic formulations intended to avoid any psychoactive impact.
Regular THC monitoring is crucial in the formulation and administration of cannabis medications. This includes third-party testing of medical cannabis products to verify THC concentrations and ensure they remain below psychoactive levels. By establishing reliable THC limits, healthcare providers can offer cannabis-based therapies with confidence that these treatments will not impair the daily functioning of patients. Especially in populations sensitive to THC, such as the elderly or individuals with mental health concerns, ensuring a non-psychoactive formulation is key to maintaining safety and efficacy in medical applications.
Additionally, patient response to low-THC or THC-free cannabis formulations should be carefully monitored to assess the effectiveness of flavonoids without psychoactive side effects. As clinical evidence on flavonoid-specific cannabis treatments grows, the development of refined, THC-free or low-THC products could provide more targeted pain relief solutions, improving quality of life for patients without exposing them to the risks associated with THC. By closely monitoring both flavonoid efficacy and THC content, medical professionals can better tailor cannabis-based pain management to patient needs, ensuring therapeutic benefits are maximized without unintended psychoactive effects.
Conclusion
In summary, the medical application of cannabis flavonoids holds significant potential for pain management, especially for patients who have not responded adequately to conventional treatments. Flavonoids, such as cannflavin A and B, exhibit notable anti-inflammatory and analgesic properties that could address chronic pain more effectively than some traditional medications. However, regulatory guidelines emphasize a cautious approach, restricting the use of cannabis-based therapies to last-resort scenarios. This helps ensure that cannabis is used responsibly and only when other treatments have been exhausted or deemed ineffective.
A major concern in medical cannabis use remains the presence of THC, the psychoactive compound in cannabis, which can impair cognitive and motor functions if not carefully regulated. To mitigate this risk, strict monitoring of THC levels in cannabis-derived treatments is essential. By setting low THC thresholds and ensuring formulations are non-psychoactive, healthcare providers can offer the benefits of cannabis flavonoids without unwanted psychoactive effects, particularly in sensitive populations such as the elderly or those with mental health issues.
Overall, the integration of cannabis flavonoids into pain management regimens provides a promising pathway, particularly as research expands our understanding of their benefits and safety. Through careful regulation, restricted use as a last resort, and rigorous THC monitoring, cannabis flavonoids can be responsibly incorporated into medical practices, offering safe and effective pain relief tailored to patients’ needs. This approach strikes a balance between innovation in pain management and a commitment to patient safety, supporting the therapeutic potential of cannabis within the medical field.