
Early 20th Century: The Decline of Cannabis in Medicine
Introduction
The early 20th century saw a significant decline in the medical use of cannabis due to political, social, and medical changes. Once widely used in pharmacopoeias, cannabis’ medical reputation diminished as evolving medical practices, regulatory shifts, and cultural attitudes raised concerns about its safety and efficacy. This summary will explore the historical role of cannabis in medicine, its uses before the decline, and the key factors that led to its reduced presence in the medical field.
Historical Background: Cannabis in Medicine Before the 20th Century
Early Global Use of Cannabis for Medical Purposes
For thousands of years, people from many cultures have utilized cannabis for medical purposes. It was first used in traditional Chinese medicine to treat conditions like pain, inflammation, and rheumatism in ancient China, when its history is first documented. Ancient civilizations such as India, Egypt, and Persia also utilized cannabis for medicinal purposes, and its use spread throughout Europe during the Middle Ages.
By the 19th century, cannabis had become a widely accepted treatment in Western medicine. In 1839, Sir William O’Shaughnessy, an Irish physician working in India, published a groundbreaking study on the medical applications of cannabis. His research demonstrated the plant’s efficacy in treating conditions such as muscle spasms, seizures, and rheumatic pain. This opened the door for cannabis to be included in various Western pharmacopoeias, including the British Pharmacopoeia and the United States Pharmacopeia.
Throughout the late 19th century, pharmaceutical companies such as Parke-Davis and Eli Lilly produced cannabis-based tinctures and extracts, which were used to treat a variety of ailments. These products were widely available and prescribed by physicians to manage pain, reduce nausea, and promote sleep. Cannabis was especially popular for conditions such as migraines, neuralgia, menstrual cramps, and asthma.
Cannabis and 19th Century Medicine
By the end of the 19th century, cannabis had established itself as a legitimate medicinal substance. It was frequently employed to treat patients suffering from chronic pain, spastic disorders, and a variety of neurological conditions. Cannabis was also used as an alternative to opiates for patients who had developed a tolerance to morphine or were at risk of addiction. The plant’s mild sedative properties made it valuable for treating insomnia and anxiety, while its analgesic effects provided relief for conditions such as arthritis and fibromyalgia.
The global demand for cannabis-based medicines led to an increase in the cultivation of the plant, with countries such as India and Egypt becoming major exporters of cannabis. Medical journals from the 19th century frequently featured case studies and reports highlighting the therapeutic benefits of cannabis, with many physicians viewing it as a versatile and effective treatment option.
However, despite its widespread use, cannabis presented several challenges. The plant’s potency could vary significantly depending on how it was prepared, making it difficult to standardize dosages. Additionally, the psychoactive effects of tetrahydrocannabinol (THC), the primary psychoactive compound in cannabis, were not well understood at the time, leading to occasional concerns about its safety. These issues, combined with broader changes in the medical field, set the stage for the eventual decline of cannabis in medicine during the early 20th century.
The Rise of Modern Medicine and the Push for Standardization

Emergence of Scientific Medicine
The turn of the 20th century marked the beginning of a new era in medicine, one that prioritized scientific rigor, standardization, and evidence-based practices. Known as the Scientific Medicine Movement, this shift was driven by advancements in medical research, the discovery of new pharmaceuticals, and a growing emphasis on the clinical testing of treatments. The movement aimed to establish a more controlled and predictable approach to medicine, with standardized treatments and dosages that could be reliably replicated.
Cannabis, with its complex chemical composition and varying effects, did not easily fit into this new paradigm. The plant contains over 100 different cannabinoids, including CBD (cannabidiol) and THC, and its effects can differ based on factors such as the strain, preparation method, and dosage. This made it difficult for physicians to prescribe cannabis with the same level of precision that was increasingly expected in modern medicine.
Pharmaceutical companies began developing synthetic drugs that could offer more consistent and predictable results. The development of aspirin in 1899, for example, provided a reliable and standardized alternative to cannabis for treating pain and inflammation. Aspirin quickly gained popularity among physicians, who appreciated its ease of use and effectiveness. As more synthetic drugs entered the market, cannabis was gradually pushed to the margins of medical practice.
Challenges in Standardizing Cannabis-Based Medicines
One of the major issues with cannabis in the early 20th century was the difficulty in standardizing its medical use. Unlike synthetic drugs, which could be manufactured with precise dosages and consistent formulations, cannabis extracts varied significantly in potency. This made it challenging for physicians to determine the appropriate dosage for patients, leading to inconsistent results.
Furthermore, cannabis-based medicines were often prepared using crude methods that did not isolate specific active compounds. While tinctures and extracts were commonly used, the varying concentration of cannabinoids, particularly THC, resulted in unpredictable effects. Patients could experience anything from mild sedation to intense psychoactive effects, depending on the dosage and preparation method.
As the medical community became more focused on precision and standardization, these inconsistencies made cannabis less appealing. Physicians began to prefer synthetic drugs that could offer consistent, controlled outcomes, reducing the risk of adverse reactions. This shift in medical practice contributed significantly to the decline of cannabis as a treatment option.
Early 20th Century Drug Regulation: The Pure Food and Drug Act of 1906
The Need for Drug Regulation
At the start of the 20th century, the medical field was grappling with the widespread availability of unregulated medicines. Many patent medicines sold during this time contained harmful or addictive substances, such as morphine, cocaine, and alcohol, without adequate labeling or oversight. As a result, there was a growing demand for federal regulation to ensure the safety and efficacy of medicines.
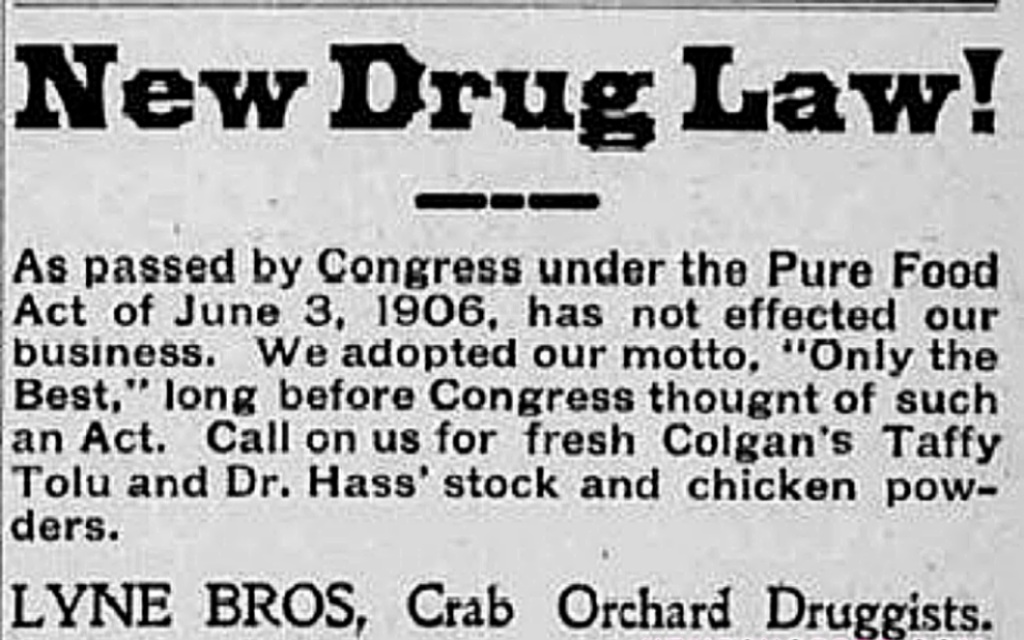
In response to these concerns, the Pure Food and Drug Act was passed in the United States in 1906. This historic law required proper ingredient labeling on foods and medications in an effort to shield customers from phony and dangerous items. The act marked the first significant step toward federal regulation of drugs, setting the stage for more comprehensive drug control measures in the decades that followed.
Impact on Cannabis-Based Medicines
While the Pure Food and Drug Act was not specifically aimed at cannabis, it had a significant impact on the availability of cannabis-based medicines. The act required that all medicines be labeled with their active ingredients, including any potentially dangerous or addictive substances. This brought attention to the psychoactive effects of THC, raising concerns about the safety of cannabis medicines.
As physicians and regulators became more aware of the psychoactive properties of cannabis, they began to view the plant with increased suspicion. The idea that cannabis could alter consciousness or induce “euphoric” effects made it less attractive to the medical community, particularly as alternatives like aspirin and barbiturates became available. The rise of the temperance movement and anti-drug campaigns further contributed to the stigmatization of cannabis, as public health advocates warned of the dangers of all psychoactive substances, regardless of their medical use.
Moral and Cultural Shifts: The Temperance Movement and Drug Stigmatization
The Temperance Movement and Cannabis
The early 20th century saw the rise of the Temperance Movement, a social campaign that aimed to reduce the consumption of alcohol and other intoxicating substances. While the movement was primarily focused on alcohol, its influence extended to other drugs, including cannabis. Temperance advocates often conflated cannabis with more dangerous substances such as opium and heroin, warning that it could lead to addiction and moral decay.
The temperance movement’s influence reached its peak with the passage of Prohibition in 1920, which banned the sale and consumption of alcohol in the United States. This cultural shift toward abstinence from intoxicating substances helped to create a climate of fear and suspicion around cannabis. Public health campaigns often painted cannabis as a dangerous drug that could lead to social ills such as crime, addiction, and mental illness.
Racialization of Cannabis and Its Impact on Medical Use
In addition to the temperance movement, the racialization of cannabis contributed to its decline in medicine. During the early 20th century, Mexican immigrants brought with them the practice of using cannabis recreationally, a practice that became associated with the term “marihuana.” As cannabis became linked with marginalized immigrant communities, it began to be viewed as a drug that threatened public safety and moral order.
Racist and xenophobic attitudes toward Mexican immigrants and other minority groups fueled anti-cannabis sentiment. Politicians and law enforcement officials used cannabis as a tool to target these communities, portraying the plant as a substance that led to deviant behavior and violence. This racialized perception of cannabis further distanced it from its medical roots, as it became associated with criminality and vice rather than legitimate medical use.
The Role of the American Medical Association (AMA)
AMA’s Skepticism Toward Cannabis
Early in the 20th century, opinions toward cannabis among the general public and professionals were greatly influenced by the American Medical Association (AMA). As the AMA became more focused on scientific rigor and evidence-based medicine, it began to question the efficacy and safety of cannabis as a treatment option. The lack of clinical trials and standardized formulations made it difficult for physicians to endorse cannabis with the same confidence as newer synthetic drugs.
By the 1930s, the AMA had become increasingly skeptical of cannabis, viewing it as a drug with limited medical value and potential for abuse. This skepticism was reinforced by the growing influence of anti-drug campaigns, which portrayed cannabis as a dangerous substance that could lead to addiction and mental illness.
AMA’s Response to Cannabis Regulation
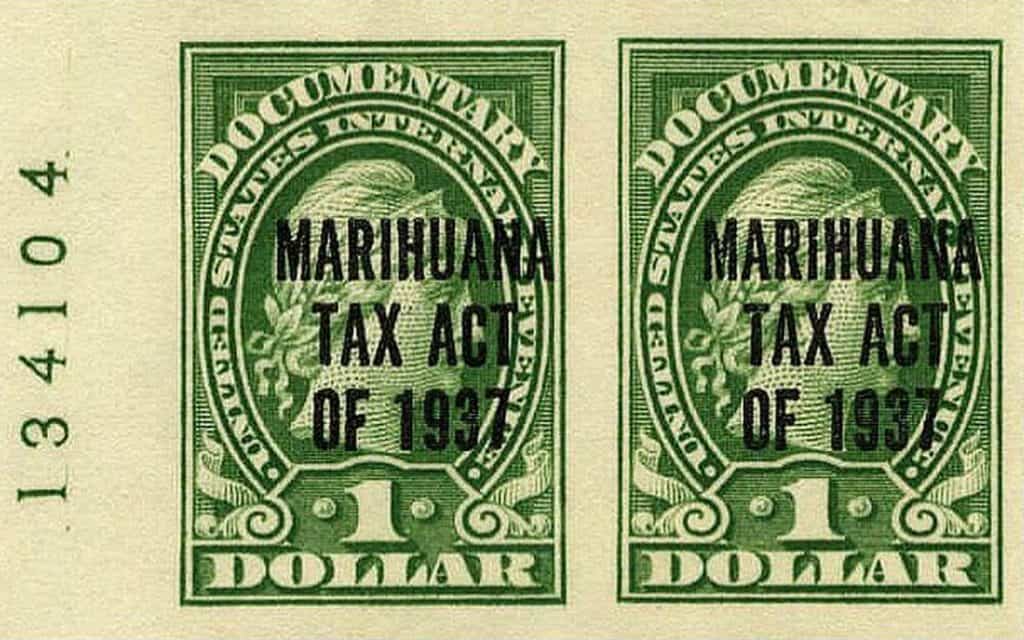
Despite its skepticism, the AMA was initially opposed to the criminalization of cannabis. In 1937, when the Marihuana Tax Act was introduced in the United States Congress, the AMA expressed concern that the law would limit physicians’ ability to prescribe cannabis for legitimate medical purposes. The AMA argued that more research was needed to determine the medical value of cannabis before it was subjected to strict regulatory controls.
However, the AMA’s opposition was ultimately ineffective, and the Marihuana Tax Act was passed in 1937. This law imposed stringent regulations on the cultivation, distribution, and possession of cannabis, making it nearly impossible for physicians to access the plant for medical use. The passage of the Marihuana Tax Act marked the beginning of cannabis’ decline from the medical field, as it became increasingly difficult for patients and physicians to obtain and use cannabis legally.
The Marihuana Tax Act of 1937 and Its Aftermath
Passage of the Marihuana Tax Act
A pivotal moment in the American cannabis industry’s history was the Marihuana Tax Act of 1937. The act placed heavy restrictions on the production, distribution, and use of cannabis, effectively criminalizing the plant. While the law did not explicitly ban medical cannabis, it imposed such strict regulations that it became nearly impossible to legally use the plant for medicinal purposes.
Under the Marihuana Tax Act, individuals who wished to cultivate or sell cannabis were required to obtain a tax stamp from the federal government. However, the process of obtaining this stamp was deliberately cumbersome and restrictive, making it difficult for anyone to comply with the law. Furthermore, the penalties for non-compliance were severe, including hefty fines and imprisonment.
Impact on Medical Cannabis
The Marihuana Tax Act had a devastating impact on the availability of cannabis-based medicines. Pharmaceutical companies, which had previously produced cannabis tinctures and extracts, ceased production due to the legal and financial risks associated with the new regulations. Physicians, who had once prescribed cannabis for a variety of ailments, no longer had access to the plant or the products derived from it.
As a result, cannabis effectively disappeared from the medical landscape in the United States. By the late 1930s, cannabis was no longer listed in the United States Pharmacopeia, and its use in medicine became a distant memory. The passage of the Marihuana Tax Act marked the beginning of cannabis’ prohibition, which would last for several decades.
International Influence: Global Decline of Medical Cannabis
Cannabis Regulation Beyond the United States
The decline of cannabis in medicine was not limited to the United States. The global influence of U.S. drug policy, combined with the rise of international drug control efforts, contributed to the worldwide suppression of medical cannabis.
In 1925, the League of Nations included cannabis in its International Opium Convention, which sought to regulate the production and distribution of narcotic drugs. Although the convention was primarily focused on opiates, cannabis was added to the list of controlled substances due to pressure from countries such as Egypt and Turkey, where cannabis use was seen as a social and public health problem.
United Nations’ Single Convention on Narcotic Drugs (1961)
The inclusion of cannabis in the International Opium Convention laid the groundwork for future international drug control efforts. Cannabis was categorized as a Schedule I narcotic in 1961 by the United Nations’ Single Convention on Narcotic Drugs, a classification designated for substances having a high potential for abuse and no established medicinal use. This international consensus on cannabis as a dangerous drug further contributed to its decline in medical use, as countries around the world adopted similar prohibitive policies.
The global regulatory framework established by the Single Convention effectively limited the availability of cannabis for medical research and therapeutic use. Countries that had previously allowed cannabis to be used in medicine were now subject to international pressure to restrict its use, contributing to the plant’s continued exclusion from mainstream medical practice.
Decline in Cannabis Research and Knowledge
Loss of Scientific Understanding
One of the most significant consequences of the decline of cannabis in medicine was the loss of scientific knowledge about the plant’s therapeutic properties. As cannabis became increasingly restricted and stigmatized, research into its medical applications came to a halt. Without access to cannabis for scientific study, researchers were unable to explore its potential benefits or develop standardized formulations that could meet the requirements of modern medicine.
This lack of research further entrenched the perception that cannabis had little to no medical value. Without new clinical evidence to support its use, cannabis was dismissed as an outdated and potentially dangerous treatment option. The scientific community largely turned its attention to synthetic drugs, leaving the study of cannabis in obscurity.
The Consequences of Research Suppression
The suppression of cannabis research had long-lasting effects on the medical field. Many of the potential therapeutic applications of cannabis, which had been identified in the 19th century, were forgotten or overlooked. Conditions that might have been treated with cannabis, such as chronic pain, epilepsy, and spastic disorders, were instead managed with synthetic pharmaceuticals that often came with their own set of risks and side effects.
The late 20th century saw the beginning of a renaissance of interest in medical cannabis. With the gradual relaxation of cannabis laws in countries such as the Netherlands and Canada, as well as in several U.S. states, researchers were once again able to investigate the plant’s medical potential. However, the legacy of cannabis’ decline in the early 20th century continued to shape the debates around its medical use.
Conclusion: The Enduring Legacy of Cannabis’ Decline in Medicine
The decline of cannabis in medicine during the early 20th century was the result of a complex interplay of factors, including the rise of scientific medicine, the development of synthetic pharmaceuticals, the influence of moral campaigns, and the implementation of strict drug regulations. Together, these forces contributed to the stigmatization of cannabis and its exclusion from mainstream medicine.
The passage of the Marihuana Tax Act of 1937 marked a turning point in the history of cannabis, as the plant was effectively criminalized and removed from medical practice. The global impact of U.S. drug policy, combined with the rise of international drug control efforts, further cemented cannabis’ decline as a therapeutic substance.
Despite this decline, cannabis’ medical potential was never entirely forgotten. In recent decades, a growing body of research has begun to re-examine the plant’s therapeutic properties, leading to a renewed interest in medical cannabis. However, the legacy of cannabis’ decline in the early 20th century continues to shape the legal and medical landscape today, as researchers and policymakers grapple with the challenges of re-integrating cannabis into modern medicine.