Table of Contents
Does marijuana cause cancer
The question of whether marijuana causes cancer is complex and nuanced, involving diverse mechanisms of action, modes of use, and the interaction of cannabinoids with cellular processes. Scientific consensus has not definitively established marijuana (cannabis) as a direct carcinogen in the way that tobacco is, but the relationship between cannabis and cancer is far from settled.
1. Understanding Marijuana’s Composition
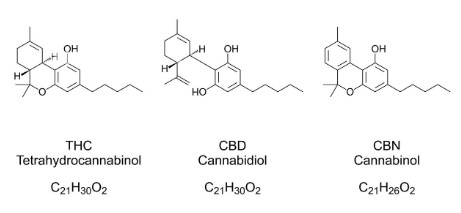
Cannabis contains over 100 biologically active cannabinoids, with Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most prominent. It also contains terpenes, flavonoids, and depending on the form of consumption combustion byproducts. These compounds vary in their biological activity, toxicity, and therapeutic potential.
a. THC and CBD Effects on Cells
- THC: Has psychoactive effects and interacts with CB1 and CB2 receptors. Some studies show THC can induce apoptosis (programmed cell death) in tumor cells, while others show it may promote angiogenesis (formation of new blood vessels), which could support tumor growth.
- CBD: Is non-psychoactive and has been shown to inhibit tumor cell proliferation, reduce inflammation, and induce apoptosis in some cancer types.
2. Routes of Exposure and Cancer Risk
The risk profile of marijuana changes significantly based on the mode of consumption.
a. Smoking Cannabis
- Combustion Risks: Smoking cannabis exposes users to many of the same carcinogens found in tobacco smoke, including polycyclic aromatic hydrocarbons (PAHs), benzene, and toluene. These compounds are known to cause mutations in DNA and promote cancer development.
- Respiratory Exposure: Chronic cannabis smokers often report symptoms of bronchitis and airway inflammation. Biopsies of cannabis smokers’ lungs sometimes show precancerous changes, although conclusive evidence linking cannabis smoking to lung cancer remains weak.

b. Vaporizing and Edibles
- Vaporizing: Avoids combustion and may reduce exposure to carcinogens, though high-temperature vaporizing can still produce some harmful substances.
- Edibles: Do not involve inhalation, significantly reducing the risk of respiratory cancers. However, systemic effects of cannabinoids on hormone-sensitive or immunologically relevant tissues remain under investigation.
3. Epidemiological Evidence on Cannabis and Cancer
The results of human studies are inconsistent, in part due to confounding variables (especially concurrent tobacco use).
a. Lung Cancer
- Mixed Evidence: Some case-control studies found no significant association between long-term cannabis smoking and lung cancer after adjusting for tobacco use. However, other studies indicate a potential increased risk, especially in heavy users.
- Limitations: Small sample sizes, self-reporting bias, and mixed tobacco/cannabis use often obscure clear conclusions.
b. Head, Neck, and Oral Cancers
- Possible Association: Some studies found elevated risks of oral cancers among cannabis users, particularly in populations where chewing or smoking cannabis is common.
- Confounders: Alcohol use, tobacco use, and HPV infections complicate interpretations.
c. Testicular Cancer
- More Consistent Signal: Several epidemiological studies have found a possible link between heavy cannabis use (especially before age 25) and increased risk of non-seminomatous testicular germ cell tumors (NS-TGCTs). This is one of the most consistently observed potential cancer risks associated with marijuana.
- Mechanism: Theories involve endocrine disruption by cannabinoids, though more mechanistic studies are needed.
d. Prostate and Bladder Cancer
- Prostate: Early evidence from small studies suggests increased expression of cannabinoid receptors in prostate cancer tissue. However, no strong link between cannabis use and increased prostate cancer incidence has been shown.
- Bladder: Some observational studies reported a decreased risk of bladder cancer among cannabis users, possibly due to anti-inflammatory effects of cannabinoids, though data are preliminary.
4. Potential Anti-Cancer Properties
Research into cannabinoids as potential anti-cancer agents is robust but largely preclinical (in vitro and animal models).
a. CBD and THC Effects
- Inhibition of Tumor Growth: In lab settings, both THC and CBD can inhibit tumor cell proliferation in gliomas, breast, prostate, and colorectal cancer cell lines.
- Mechanisms:
- Induction of apoptosis
- Inhibition of angiogenesis
- Suppression of metastasis
- Reduction of oxidative stress
b. Synergistic Effects with Chemotherapy
Cannabinoids may enhance the effects of chemotherapy in some settings or reduce tumor resistance to chemotherapy. However, in other cases, cannabinoids may interfere with chemotherapeutic drug metabolism, highlighting the need for caution and further research.
5. Immunomodulation and Cancer Susceptibility
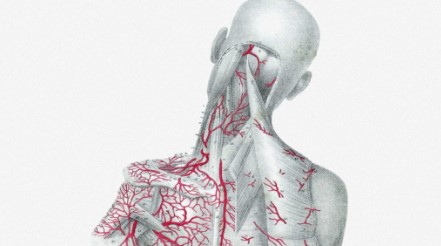
Cannabinoids are known to modulate the immune system, which could influence cancer risk.
- Immunosuppressive Effects: THC can suppress T-cell activation, reduce cytokine production, and alter macrophage activity, potentially impairing the body’s natural cancer surveillance.
- Chronic Use: In immunocompromised individuals (e.g., HIV patients, transplant recipients), long-term cannabis use could theoretically reduce the ability to detect and destroy early neoplastic cells.
6. Comparison to Tobacco
While cannabis and tobacco both produce harmful combustion byproducts, the patterns of use differ significantly:
- Frequency: Cannabis users often smoke fewer joints per day compared to the number of cigarettes smoked by tobacco users.
- Filter and Paper Differences: Cannabis is often smoked without filters and held in the lungs longer, potentially increasing exposure per puff.
- Co-use: Many cannabis users also smoke tobacco, making it difficult to isolate cannabis-specific risks.
7. Cannabis Use in Cancer Patients
Cannabis is increasingly used by cancer patients for symptom management.
a. Palliative Benefits
- Nausea and Vomiting: THC has been approved in synthetic form (dronabinol) to treat chemotherapy-induced nausea and vomiting.
- Pain: Cannabis may help with neuropathic and cancer-related pain, especially where opioids are inadequate.
- Appetite: Cannabinoids can stimulate appetite, beneficial in patients experiencing cachexia or anorexia.
b. Risks in Immunocompromised Patients
- Infectious Risk: Inhaled cannabis may introduce fungal pathogens such as Aspergillus, a concern in neutropenic patients.
- Psychiatric Side Effects: Cancer patients vulnerable to anxiety or depression may be adversely affected by THC, especially at high doses.
8. Regulatory and Research Challenges
Due to its Schedule I status in many jurisdictions, research on cannabis has been historically restricted. This has limited large-scale, controlled trials that could clarify long-term risks.
- Need for Longitudinal Studies: Most data comes from small, retrospective studies or animal models.
- Standardization Issues: Varying THC/CBD ratios, routes of administration, and dosing further complicate risk assessment.
Conclusion
At present, the evidence that marijuana causes cancer is inconclusive but cautionary. While smoking cannabis introduces known carcinogens into the respiratory tract, large-scale epidemiological studies have not definitively shown a strong link between marijuana use and most cancers. The most consistent association is with testicular cancer, particularly in heavy, early-onset users.
Conversely, cannabinoids, particularly CBD, show promising anti-cancer effects in preclinical models. Cannabis also has clear palliative benefits for many cancer patients. The complex interplay between therapeutic and potentially harmful effects of cannabinoids requires more comprehensive clinical studies to untangle.
For now, minimizing combustion-based consumption, moderating use, and being aware of risk factors (e.g., immunosuppression, co-use with tobacco) are prudent measures for users concerned about long-term cancer risk.