
CBD vs THC: What’s the Difference in the Medical Field?
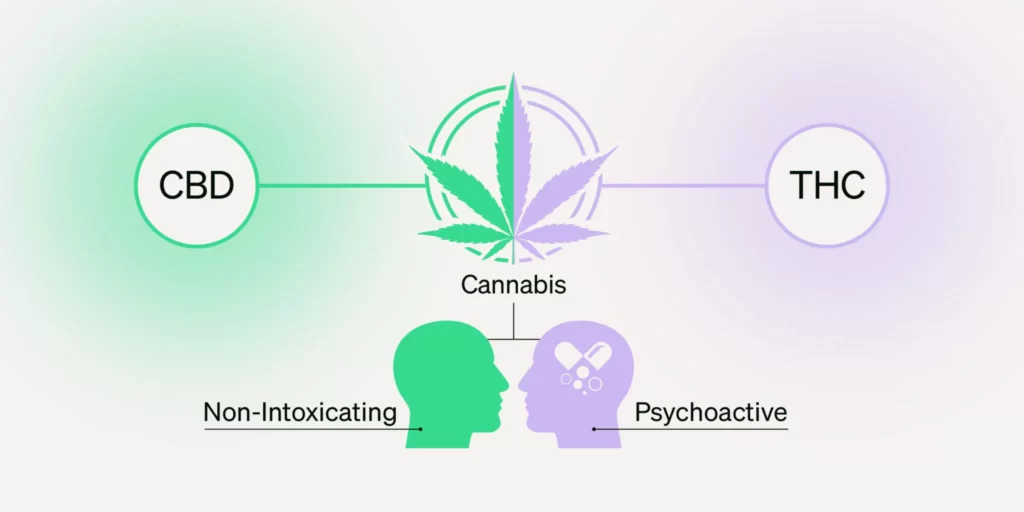
Cannabis has long been used for medicinal purposes, but its widespread application in the modern medical field is largely attributed to two primary cannabinoids: Cannabidiol (CBD) and Tetrahydrocannabinol (THC). Both CBD and THC interact with the body’s endocannabinoid system (ECS), but their effects, applications, and legal status in the medical world vary significantly. Understanding the medical implications of both cannabinoids is crucial for healthcare professionals, patients, and researchers. This detailed analysis focuses exclusively on the medical use of CBD and THC, explaining their differences, benefits, and limitations.
Understanding Cannabinoids and the Endocannabinoid System
Before diving into the differences between CBD and THC, it’s essential to understand their role as cannabinoids. Chemical substances called cannabinoids have an effect on the human body’s endocannabinoid system (ECS). ECS components include endogenous cannabinoids, enzymes, and cannabinoid receptors (CB1 and CB2). This system regulates various physiological functions, including mood, pain, appetite, and immune responses.
The two most common cannabinoids in cannabis plants are THC and CBD. While both interact with the ECS, their effects on the body differ due to how they interact with cannabinoid receptors.
- CBD (Cannabidiol): Primarily interacts with CB2 receptors found in immune tissues, influencing anti-inflammatory responses and other regulatory functions.
- THC (Tetrahydrocannabinol): Binds primarily to CB1 receptors, which are highly concentrated in the brain and central nervous system. THC is psychoactive and induces changes in perception, mood, and cognition.
Chemical Structure and Functionality of CBD vs THC
Both CBD and THC share a similar molecular structure: 21 carbon atoms, 30 hydrogen atoms, and 2 oxygen atoms. Despite this similarity, the arrangement of atoms in each cannabinoid differs, which leads to distinct effects on the body.
- CBD (Cannabidiol):
- Non-psychoactive.
- Does not directly bind to CB1 receptors.
- Modulates the ECS by inhibiting the enzyme FAAH, which breaks down anandamide (a natural cannabinoid produced by the body).
- Indirectly impacts CB2 receptors, contributing to its anti-inflammatory, anti-anxiety, and neuroprotective properties.
- THC (Tetrahydrocannabinol):
- Psychoactive.
- Binds directly to CB1 receptors in the brain and central nervous system.
- Responsible for the “high” associated with cannabis use.
- THC’s medical applications include pain relief, appetite stimulation, and anti-nausea effects.
The Medical Benefits of CBD

CBD has gained popularity in the medical field due to its wide range of therapeutic benefits without inducing psychoactive effects. The following are some key medical applications of CBD:
1. Pain Management
One of the primary medical uses of CBD is its ability to manage chronic pain. CBD modulates pain through its interaction with CB2 receptors, which regulate inflammatory responses. In conditions such as arthritis, multiple sclerosis, and fibromyalgia, patients have reported significant reductions in pain after using CBD-based medications.
Clinical Studies:
- A study published in the European Journal of Pain demonstrated that CBD can help lower pain and inflammation in animal models of arthritis.
- In human trials, CBD has been shown to provide relief for chronic pain without the side effects commonly associated with opioids.
2. Anti-inflammatory Properties
CBD’s interaction with CB2 receptors makes it a potent anti-inflammatory agent. It has been found to reduce inflammation in a variety of medical conditions, including inflammatory bowel disease (IBD), Crohn’s disease, and other autoimmune disorders.
Medical Application:
- In diseases where chronic inflammation is a significant problem, such as in cardiovascular diseases or neurodegenerative disorders, CBD helps by reducing inflammatory markers.
3. Anxiety and Depression
CBD’s impact on mental health has been well-documented, particularly its ability to reduce anxiety and depression without the side effects of traditional pharmaceuticals. CBD’s interaction with serotonin receptors (5-HT1A) in the brain plays a role in mood regulation, reducing anxiety and stress responses.
Clinical Evidence:
- Studies have found that patients with generalized anxiety disorder, social anxiety, and PTSD experience relief with regular CBD use.
- CBD’s non-habit-forming nature makes it an ideal alternative for patients who cannot tolerate or become dependent on traditional anti-anxiety medications.
4. Epilepsy and Seizures
One of the most notable successes of CBD in the medical field is its effectiveness in treating epilepsy. In particular, CBD has been approved for use in managing Dravet syndrome and Lennox-Gastaut syndrome, two rare and severe forms of epilepsy.
FDA Approval:
- The first FDA-approved medicine for treating seizures brought on by these diseases is Epidiolex, a CBD-based product. It has shown significant success in reducing seizure frequency.
5. Neuroprotective Effects
CBD’s potential as a neuroprotective agent has made it a subject of interest in treating neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and Huntington’s disease. By reducing oxidative stress and inflammation in the brain, CBD protects neurons from damage.
Current Research:
- Animal studies have shown that CBD may help slow the progression of neurodegenerative diseases. Trials in humans are being conducted to find out how effective it is.
The Medical Benefits of THC

While THC is often associated with its psychoactive effects, its medical applications are significant and have been recognized in various therapeutic contexts. The following are some of the key medical uses of THC:
1. Chronic Pain Relief
THC’s ability to bind to CB1 receptors makes it effective in managing pain, particularly in conditions such as neuropathy, cancer pain, and pain associated with spinal cord injuries. Unlike CBD, which modulates pain through inflammation, THC directly alters the brain’s perception of pain.
Medical Application:
- In cancer patients undergoing chemotherapy, THC is often used to alleviate pain that does not respond to standard analgesics.
- THC-containing medications, such as Marinol (dronabinol), have been approved by the FDA for pain relief in cancer and AIDS patients.
2. Appetite Stimulation
THC has long been used to stimulate appetite in patients with conditions that lead to severe weight loss, such as cancer, HIV/AIDS, and eating disorders. By interacting with CB1 receptors, THC enhances the release of hormones that promote hunger.
Approved Use:
- THC is used in palliative care to improve the quality of life for terminally ill patients by increasing appetite and reducing nausea.
3. Nausea and Vomiting
THC is effective in controlling nausea and vomiting, particularly in cancer patients undergoing chemotherapy. Its anti-emetic properties are among the most well-researched, and THC-based medications have been widely prescribed for this purpose.
FDA Approval:
- Cesamet (nabilone), a synthetic cannabinoid that mimics the effects of THC, is FDA-approved for treating nausea and vomiting caused by chemotherapy.
4. Muscle Spasticity
THC has shown significant efficacy in treating muscle spasticity, particularly in patients with multiple sclerosis (MS). Muscle spasticity leads to stiffness and muscle tightness, often causing pain and mobility issues. THC’s muscle relaxant properties provide relief from these symptoms.
Clinical Trials:
- Studies have demonstrated that THC reduces spasticity and improves mobility in patients with MS, leading to an improved quality of life.
5. Glaucoma
Although newer treatments have become more common, THC was once widely used to reduce intraocular pressure in glaucoma patients. By dilating blood vessels and reducing pressure inside the eye, THC helped manage the symptoms of this condition.
Current Use:
- While not as commonly prescribed as it once was, THC remains a potential treatment for patients who are unresponsive to other glaucoma therapies.
Key Differences Between CBD and THC in the Medical Field
Despite both cannabinoids being derived from the same plant, CBD and THC differ significantly in terms of their medical applications, side effects, and legality.
1. Psychoactivity
The most significant difference between CBD and THC is that THC is psychoactive, while CBD is not. This distinction is critical in the medical field, as CBD can be used without altering a patient’s mental state. THC’s psychoactivity, however, limits its use in patients who may not tolerate cognitive changes or who are susceptible to psychotic episodes.
2. Legal Status
CBD and THC have different legal statuses across the globe. CBD is legal in many countries and U.S. states for medical purposes due to its non-psychoactive nature. In contrast, THC remains illegal in many jurisdictions due to its psychoactive effects, although it is approved for medical use in several places under strict regulations.
Examples:
- THC is listed as a Schedule I drug under the Controlled Substances Act, whereas CBD made from hemp that has less than 0.3% THC is allowed on a federal level in the United States.
- Countries such as Canada and Uruguay have legalized both CBD and THC for medical purposes, with specific guidelines for their medical use.
3. Side Effects
CBD is well-tolerated with minimal side effects, even in high doses. The most common side effects include drowsiness, dry mouth, and interactions with certain medications. THC, on the other hand, can induce a range of side effects, particularly at high doses, including dizziness, increased heart rate, impaired memory, and anxiety.
Medical Consideration:
- For patients who require cannabinoid treatment but are sensitive to THC’s side effects, CBD offers a viable alternative with fewer risks.
4. Therapeutic Uses
While both cannabinoids are effective in managing pain, inflammation, and neurological disorders, they do so through different mechanisms. CBD is more suitable for patients with inflammatory and autoimmune conditions, anxiety, and seizure disorders, while THC is more effective for conditions that require appetite stimulation, nausea control, and muscle relaxation.
Combination Therapy:
- In some cases, the combination of both CBD and THC has been shown to provide a synergistic effect, where both cannabinoids work together to enhance therapeutic outcomes. This is seen in the use of Sativex, a combination of THC and CBD, which is approved for use in MS patients for the treatment of spasticity.
Restrictions on Using CBD and THC in the Medical Field as a Last Resort: Monitoring THC Levels to Prevent Psychoactive Effects
In the medical field, both CBD (Cannabidiol) and THC (Tetrahydrocannabinol) have become increasingly recognized for their therapeutic potential in treating a wide range of conditions. However, given the psychoactive properties of THC, the use of these cannabinoids—particularly THC—comes with restrictions, especially when used as a last resort. Medical professionals and regulatory bodies have implemented strict guidelines to ensure that the administration of these compounds is safe, effective, and minimizes psychoactive effects on patients.
1. Definition of “Last Resort” in the Medical Field
In medical contexts, a treatment is considered a “last resort” when all other conventional therapies have failed or have been deemed unsuitable for the patient. When it comes to using cannabinoids like CBD and THC, their designation as a last resort often occurs in situations such as:
- Chronic pain unresponsive to standard analgesics, including opioids.
- Neurological conditions like epilepsy, where traditional anti-seizure medications are ineffective.
- Chemotherapy-induced nausea and vomiting that do not respond to standard anti-emetic treatments.
- Treatment-resistant anxiety or PTSD that fails to improve with traditional antidepressants or anti-anxiety medications.
In these cases, the potential benefits of cannabinoids may outweigh the risks, but their use must still be carefully monitored to avoid adverse effects, particularly the psychoactive effects of THC.
2. Restrictions on the Use of CBD in the Medical Field
CBD, being non-psychoactive, faces fewer restrictions compared to THC. However, there are still limitations imposed by regulatory agencies to ensure safety, efficacy, and quality control in medical applications.
- Regulation of CBD-Derived Products: Many countries and regions require CBD to be derived from hemp rather than marijuana, as hemp contains very low levels of THC (typically less than 0.3%). This ensures that patients using CBD are not inadvertently exposed to high THC levels, which could cause psychoactive effects.
- Dosage Restrictions: Medical institutions often set guidelines regarding the maximum allowable doses of CBD, particularly for certain patient populations like children, pregnant women, and individuals with severe medical conditions. These restrictions help prevent potential side effects, such as drug interactions, sedation, or liver enzyme disturbances, which may occur at high doses.
- CBD as an Adjunctive Therapy: CBD is often used in combination with other medications to enhance therapeutic effects. However, healthcare providers must ensure that CBD does not interact with other medications in ways that could compromise patient safety. For instance, CBD can inhibit the cytochrome P450 enzyme system, which is responsible for metabolizing many medications, potentially leading to altered drug levels in the bloodstream.
3. Restrictions on the Use of THC in the Medical Field
The use of THC in medical treatments is subject to much stricter regulations due to its psychoactive properties. The primary concern with THC is its potential to cause euphoria, cognitive impairment, and, in some cases, anxiety or paranoia. For this reason, the medical community implements several layers of restrictions to ensure that THC is only used when necessary and that its psychoactive effects are minimized.
Legal Restrictions
- Controlled Substance Classification: In many countries, THC is classified as a controlled substance. For instance, THC is classified as a Schedule I drug in the US under the Controlled Substances Act, which means that there is no recognized federal medicinal use for it and a significant potential for misuse (though some states may permit medical usage under certain circumstances). Patients and healthcare providers must navigate complex legal frameworks to prescribe or administer THC-based treatments.
- Medical Cannabis Programs: In regions where THC is legal for medical use, it is typically available only through tightly regulated medical cannabis programs. These programs require patients to obtain a medical cannabis card or recommendation from a certified healthcare provider. Patients must meet specific criteria—such as having a qualifying condition like cancer, epilepsy, or chronic pain—to access THC-based medications.
Dosage and Administration Restrictions
- Limitations on THC Concentrations: To prevent excessive psychoactive effects, medical regulators often impose strict limits on the concentration of THC in cannabis-based medications. In many jurisdictions, the allowable THC concentration in medical products is capped at a specific percentage. For example, products containing more than 5-10% THC may be restricted to severe cases or special circumstances.
- Dosing Guidelines: Healthcare providers are required to follow strict dosing guidelines when prescribing THC. Starting with the lowest effective dose is standard practice, and the dosage may be titrated based on the patient’s response. This approach helps minimize the psychoactive effects while providing therapeutic relief. Physicians may also recommend formulations with balanced ratios of CBD and THC, as the presence of CBD can modulate and reduce the psychoactivity of THC.
Restrictions on Patient Populations
- Vulnerable Populations: The use of THC is heavily restricted in certain patient populations, including children, adolescents, the elderly, pregnant or breastfeeding women, and individuals with a history of mental illness or substance use disorders. In these populations, the risk of negative psychoactive effects is higher, and alternatives like CBD or other non-cannabinoid medications may be recommended instead.
4. Monitoring THC Levels in Medications to Prevent Psychoactive Effects
Given the psychoactive nature of THC, careful monitoring of THC levels in cannabis-based medications is critical to preventing unwanted cognitive and psychological effects. This is particularly important in the medical field, where patients may be vulnerable to negative outcomes from psychoactive substances.
THC/CBD Ratio in Formulations
One of the most effective ways to monitor and control the psychoactive effects of THC is by adjusting the ratio of THC to CBD in medical formulations. Since CBD can counteract some of the psychoactive effects of THC, formulations with higher levels of CBD relative to THC are commonly prescribed in medical contexts. These balanced or CBD-dominant formulations help ensure that patients receive the therapeutic benefits of THC without experiencing excessive euphoria or cognitive impairment.
Pharmacokinetics and Therapeutic Monitoring
- Blood THC Level Monitoring: In some cases, particularly for patients receiving high doses of THC for conditions like chronic pain or chemotherapy-induced nausea, healthcare providers may monitor blood THC levels to ensure that the drug remains within therapeutic ranges. This is especially important for patients who may be at risk of cognitive impairment, as maintaining optimal THC concentrations can prevent psychoactive effects from becoming problematic.
- Controlled Release Formulations: Some medical THC products are designed to release the cannabinoid slowly over time, reducing the likelihood of a sudden spike in THC levels that could lead to psychoactive effects. These controlled-release formulations are especially useful for managing chronic conditions where long-term symptom control is necessary.
Product Testing and Labeling Requirements
- Cannabinoid Potency Testing: In most jurisdictions where medical cannabis is legal, THC-containing products must undergo rigorous potency testing to ensure that the labeled THC content matches the actual content. This testing helps ensure that patients and healthcare providers can accurately gauge how much THC a patient is ingesting, thereby minimizing the risk of unintended psychoactive effects.
- Labeling Regulations: Medical cannabis products must be clearly labeled with the concentration of THC and other cannabinoids. This transparency is critical for patients and healthcare providers to make informed decisions about dosing and to avoid overexposure to THC.
5. Alternative Cannabinoid Formulations to Reduce THC Exposure
For patients who may benefit from the therapeutic effects of THC but are at risk for negative psychoactive effects, healthcare providers can explore alternative cannabinoid formulations that minimize THC exposure while still providing therapeutic benefits.
CBD-Dominant Strains
In medical cannabis products derived from whole-plant cannabis, strains that are dominant in CBD but contain small amounts of THC are often used. These strains leverage the entourage effect, where the presence of multiple cannabinoids and terpenes enhances therapeutic efficacy. However, the high levels of CBD ensure that the psychoactive effects of THC are negligible or absent.
Synthetic Cannabinoids
- Dronabinol (Marinol) and Nabilone (Cesamet) are synthetic cannabinoids that mimic the effects of THC but have more predictable pharmacokinetics. These synthetic versions can be dosed more precisely, which helps in reducing the risk of psychoactive effects. They are FDA-approved for specific conditions such as chemotherapy-induced nausea and appetite stimulation in AIDS patients.
- Nabiximols (Sativex), a pharmaceutical-grade cannabis extract, contains both THC and CBD in a balanced formulation. It is often prescribed to patients with multiple sclerosis for muscle spasticity, providing therapeutic benefits without overwhelming psychoactive effects due to the balancing role of CBD.
6. Medical Oversight and Patient Education
Given the complexities of using THC in a medical context, ongoing medical oversight and patient education are vital components of treatment plans that include cannabinoids.
Role of Healthcare Providers
Healthcare providers must assess the individual needs of each patient, weighing the potential benefits of THC against the risks of psychoactive effects. For some patients, the benefits may outweigh the risks, while for others, alternative therapies may be more appropriate.
Patient Monitoring: In cases where THC is prescribed, patients should be closely monitored for signs of cognitive impairment, mood changes, or other psychoactive effects. Adjusting the dosage or switching to a different cannabinoid formulation may be necessary if these effects become problematic.
Patient Education
Educating patients about the potential psychoactive effects of THC is essential, especially when using cannabis-based medications as a last resort. Patients should be made aware of:
- The importance of adhering to prescribed dosages.
- How to recognize signs of overexposure to THC, such as dizziness, confusion, or mood changes.
- The importance of avoiding activities like driving or operating heavy machinery while taking THC-containing medications.
Conclusion
The medical use of CBD and THC represents a significant advancement in the treatment of various conditions, particularly those that are resistant to conventional therapies. However, given the unique properties and effects of each cannabinoid, there are essential distinctions and restrictions that must be considered to ensure safe and effective treatment.
CBD is widely favored in the medical field for its non-psychoactive nature, broad therapeutic potential, and low risk of side effects. Its applications in managing pain, inflammation, anxiety, epilepsy, and neurodegenerative diseases make it a valuable tool for healthcare providers. The limited restrictions on CBD, primarily related to dosage and potential drug interactions, allow for its flexible use across various patient populations. Its lack of psychoactivity makes CBD an excellent option for patients who need relief without cognitive impairment.
On the other hand, THC offers potent therapeutic benefits in areas such as chronic pain management, appetite stimulation, nausea control, and muscle spasticity relief. However, due to its psychoactive effects, the use of THC in the medical field is subject to much stricter regulations and oversight. THC’s legal status varies widely across jurisdictions, and its potential to induce cognitive and psychological side effects necessitates careful monitoring. Healthcare providers must adhere to strict dosing guidelines and monitor patients for any signs of THC-related impairment, particularly in vulnerable populations.
Monitoring THC levels in medical formulations is crucial to prevent psychoactive effects in patients. Approaches such as using controlled-release formulations, balanced THC/CBD ratios, and regular blood level monitoring help mitigate the risks associated with THC use. Additionally, product testing and clear labeling of cannabinoid concentrations ensure that both patients and healthcare providers can manage dosages safely and effectively.
In cases where CBD or THC is used as a last resort, healthcare providers must carefully weigh the benefits against the risks. The decision to use these cannabinoids typically arises when other treatments have failed, and the potential relief they offer outweighs the possible side effects. Nevertheless, the medical community has implemented clear restrictions, particularly concerning THC, to minimize risks and protect patient safety.
Finally, patient education and medical oversight are critical components in the successful use of CBD and THC in the medical field. Patients must be informed of the potential effects of these cannabinoids, especially THC, and healthcare providers must maintain ongoing monitoring and support throughout the treatment process. The focus on non-recreational, strictly medical use ensures that these compounds are leveraged to improve patient outcomes without compromising safety or well-being.
In conclusion, CBD and THC have proven to be valuable therapeutic tools in the medical field. Their differences in psychoactivity, legal status, and side effects require careful consideration when determining appropriate treatment protocols. Healthcare practitioners can guarantee that patients obtain the therapeutic benefits of cannabis while reducing undesirable euphoric effects by following set guidelines and keeping an eye on THC levels in drugs. The use of CBD and THC in medicine is anticipated to grow as research and legislation change, providing patients with diseases that were previously incurable with fresh hope.