Cannabis and Neurological Disorders: A Comprehensive Overview
Cannabis, a plant that has been used for medicinal purposes for thousands of years, has recently garnered significant attention for its potential therapeutic benefits, especially in the field of neurology. With the legalization of cannabis in many parts of the world and a surge in scientific research, there is growing evidence to suggest that cannabis and its compounds can be effective in managing various neurological disorders. This comprehensive overview aims to delve into the relationship between cannabis and neurological disorders, exploring the mechanisms, therapeutic potential, and the challenges associated with its use.
The Endocannabinoid System
To understand how cannabis affects neurological disorders, it is essential to first grasp the functioning of the endocannabinoid system (ECS). The early 1990s led to the discovery of the complex cell-signaling system known as the ECS, which is made up of receptors, enzymes, and endocannabinoids. It plays a critical role in regulating a range of physiological processes, including mood, memory, pain, and neuroprotection.
Components of the Endocannabinoid System
The ECS comprises three main components: cannabinoid receptors, endocannabinoids, and the enzymes that produce and break down endocannabinoids.
1. Endocannabinoids
Endocannabinoids are lipid-based neurotransmitters that are produced endogenously (within the body). They bind to cannabinoid receptors to exert their effects. The two primary endocannabinoids are:
- Anandamide (AEA): A common moniker for anandamide is the “bliss molecule,” derived from the Sanskrit word for bliss, “ananda.” Mood, pain, hunger, and memory are all regulated by it. Anandamide is synthesized from N-arachidonoyl phosphatidylethanolamine (NAPE) through enzymatic action and is degraded by fatty acid amide hydrolase (FAAH).
- 2-Arachidonoylglycerol (2-AG): This endocannabinoid is present at higher levels in the brain than anandamide and is involved in regulating immune function, inflammation, and neural communication. 2-AG is synthesized from diacylglycerol (DAG) by the enzyme diacylglycerol lipase (DAGL) and is degraded by monoacylglycerol lipase (MAGL).
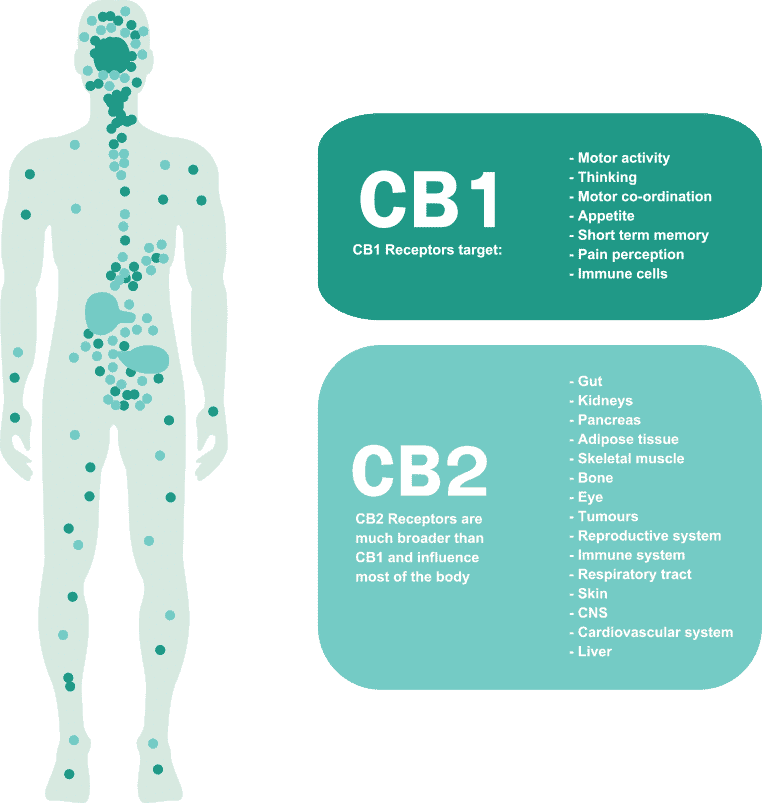
2. Cannabinoid Receptors
Cannabinoid receptors are G-protein-coupled receptors (GPCRs) located throughout the body. The two primary cannabinoid receptors are:
- CB1 Receptors: These receptors are predominantly found in the central nervous system (CNS), including the brain and spinal cord. They are highly concentrated in areas associated with cognitive function, memory, motor control, and pain sensation, such as the hippocampus, basal ganglia, and cerebellum. In addition to mediating THC’s euphoric effects, CB1 receptors are essential for controlling the release of neurotransmitters.
- CB2 Receptors: CB2 receptors are primarily located in the peripheral nervous system and immune cells, such as the spleen and white blood cells. They are involved in regulating immune function, inflammation, and pain. Activation of CB2 receptors does not produce psychoactive effects, making them a target for anti-inflammatory and analgesic therapies.
3. Enzymes
The ECS includes enzymes responsible for the biosynthesis and degradation of endocannabinoids. These enzymes ensure that endocannabinoid signaling is tightly regulated and occurs only when needed.
- FAAH (Fatty Acid Amide Hydrolase): FAAH is the enzyme responsible for degrading anandamide. Inhibiting FAAH can increase anandamide levels, potentially enhancing its therapeutic effects.
- MAGL (Monoacylglycerol Lipase): MAGL degrades 2-AG. Inhibition of MAGL can increase 2-AG levels, which may have beneficial effects in conditions involving inflammation and pain.
Cannabinoids and Their Mechanisms of Action
There are more than 100 cannabinoids in cannabis, the most researched of which being tetrahydrocannabinol (THC) and cannabidiol (CBD). These cannabinoids interact with the ECS, producing various effects.
- THC: The psychoactive component of cannabis, THC primarily binds to CB1 receptors in the brain, leading to altered perception, mood changes, and pain relief. It also has neuroprotective and anti-inflammatory properties.
- CBD: Non-psychoactive and known for its therapeutic benefits, CBD interacts with multiple receptors, including CB1, CB2, serotonin, and vanilloid receptors. It modulates the ECS indirectly and has anti-inflammatory, anxiolytic, and anticonvulsant properties.
Cannabis and Specific Neurological Disorders
1. Epilepsy
Overview
Epilepsy is a long-term neurological condition marked by frequent, spontaneous seizures brought on by aberrant brain electrical activity. Traditional antiepileptic drugs (AEDs) are the primary treatment, but approximately one-third of patients are resistant to these medications. This has led to an exploration of alternative therapies, including cannabis and its compounds.
Cannabinoids and Epilepsy
- CBD (Cannabidiol): CBD has garnered the most attention for its anticonvulsant properties. Clinical trials, particularly in pediatric epilepsy, have shown promising results. Treatment for two severe forms of epilepsy, Dravet syndrome and Lennox-Gastaut syndrome, is provided by the FDA-approved CBD extract product Epidiolex.
- THC (Tetrahydrocannabinol): THC also exhibits anticonvulsant properties but is less favored due to its psychoactive effects. However, some studies suggest that THC may be beneficial in certain types of epilepsy, particularly when used in combination with CBD.
Mechanisms of Action
- Modulation of Ion Channels: CBD can modulate ion channels involved in neuronal excitability, reducing the likelihood of seizure activity.
- GABAergic System: CBD enhances the inhibitory effects of the GABAergic system, helping to balance excitatory and inhibitory signals in the brain.
- Anti-inflammatory Effects: Both CBD and THC have anti-inflammatory properties, which can reduce neuroinflammation associated with seizure activity.
Clinical Evidence
- Clinical Trials: Numerous studies have demonstrated the efficacy of CBD in reducing seizure frequency. For example, a critical study that was published in the New England Journal of Medicine demonstrated that patients with Dravet syndrome who received CBD treatment experienced a considerable decrease in the frequency of seizures.
- Patient Reports: Anecdotal evidence from patients and caregivers also supports the use of cannabis, particularly CBD, in managing epilepsy.
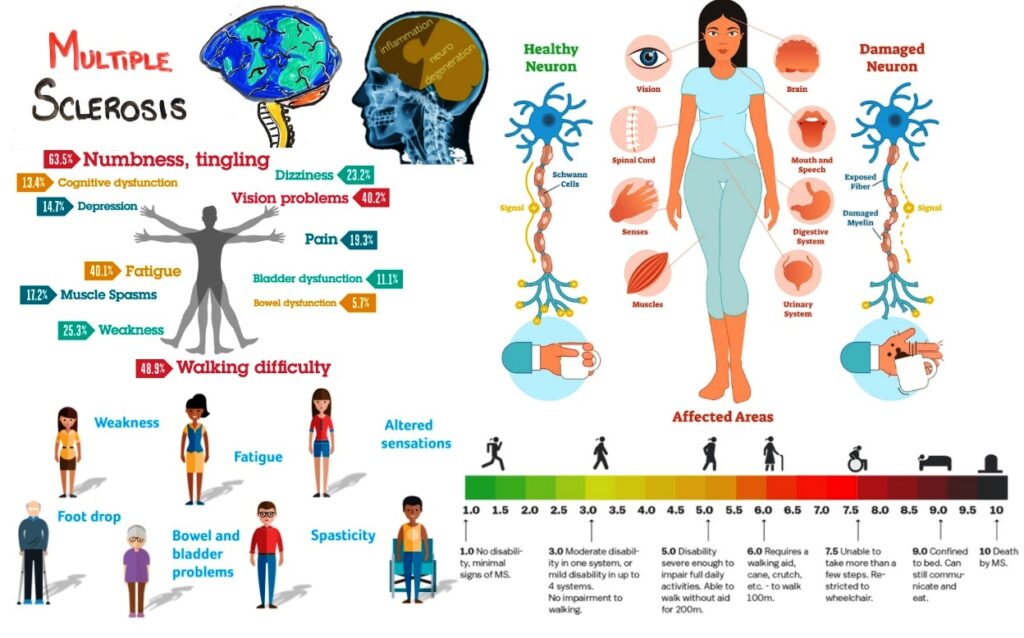
2. Multiple Sclerosis (MS)
Overview
Multiple sclerosis (MS) is an autoimmune disorder characterized by demyelination of nerve fibers in the CNS, leading to symptoms such as muscle spasticity, pain, fatigue, and cognitive impairment.
Cannabinoids and MS
- Sativex (Nabiximols): An oromucosal spray containing THC and CBD, Sativex is approved in several countries for treating spasticity and neuropathic pain in MS patients.
- CBD: Known for its anti-inflammatory and neuroprotective properties, CBD is being explored for its potential to alleviate MS symptoms without the psychoactive effects of THC.
Mechanisms of Action
- Anti-inflammatory Effects: Cannabinoids can modulate the immune response, reducing the inflammation and autoimmune activity that contribute to MS progression.
- Neuroprotection: Both CBD and THC exhibit neuroprotective properties, potentially slowing the neurodegenerative processes in MS.
- Muscle Relaxation: Activation of cannabinoid receptors can reduce muscle spasticity and improve mobility.
Clinical Evidence
- Clinical Trials: A study published in The Lancet found that Sativex significantly reduced muscle spasticity in MS patients who were unresponsive to conventional treatments .
- Patient Reports: Many MS patients report significant relief from spasticity, pain, and sleep disturbances when using cannabis-based therapies.
3. Parkinson’s Disease (PD)
Overview
The loss of dopaminergic neurons in the substantia nigra causes Parkinson’s disease (PD), a progressive neurodegenerative condition that manifests as tremors, stiffness, bradykinesia, and postural instability.
Cannabinoids and PD
- THC: Has been shown to reduce tremors and improve sleep quality in PD patients.
- CBD: May help alleviate non-motor symptoms such as psychosis, anxiety, and sleep disturbances.
Mechanisms of Action
- Modulation of Dopamine: Cannabinoids may help modulate dopamine levels in the brain, alleviating motor symptoms of PD.
- Neuroprotection: CBD and THC have neuroprotective effects, potentially slowing the progression of neuronal degeneration.
- Anti-inflammatory Effects: Reducing neuroinflammation can mitigate some symptoms and progression of PD.
Clinical Evidence
- Clinical Trials: An open-label study indicated that cannabis use improved motor and non-motor symptoms in PD patients .
- Patient Reports: Many patients report improvements in sleep, tremors, and overall quality of life when using cannabis-based treatments.
4. Alzheimer’s Disease (AD)
Overview
Alzheimer’s disease (AD) is a neurological condition marked by gradual behavioral abnormalities, memory loss, and cognitive impairment. It is linked to the buildup of tau tangles and amyloid-beta plaques in the brain.
Cannabinoids and AD
- CBD: Exhibits potential in reducing neuroinflammation, oxidative stress, and amyloid-beta accumulation.
- THC: May help improve symptoms such as agitation and sleep disturbances in AD patients.
Mechanisms of Action
- Reduction of Amyloid-Beta Plaques: Studies suggest that cannabinoids can reduce the accumulation of amyloid-beta plaques, which are characteristic of AD.
- Anti-inflammatory and Antioxidant Effects: CBD and THC can reduce neuroinflammation and oxidative stress, protecting neurons from damage.
- Modulation of Neurotransmitters: Cannabinoids may help balance neurotransmitter levels, improving cognitive function and mood.
Clinical Evidence
- Preclinical Studies: Animal studies have shown that cannabinoids can reduce amyloid-beta levels and improve cognitive function .
- Patient Reports: Anecdotal evidence suggests that cannabis may help with symptoms such as agitation, aggression, and insomnia in AD patients.
5. Amyotrophic Lateral Sclerosis (ALS)
Overview
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease that affects motor neurons, leading to muscle weakness, atrophy, and eventually respiratory failure.
Cannabinoids and ALS
- CBD and THC: Both cannabinoids may help manage symptoms such as spasticity, pain, and appetite loss. They may also offer neuroprotective benefits.
Mechanisms of Action
- Neuroprotection: Cannabinoids can protect motor neurons from degeneration, potentially slowing disease progression.
- Anti-inflammatory Effects: Reducing neuroinflammation can mitigate some symptoms of ALS.
- Symptom Management: Cannabinoids can alleviate spasticity, pain, and improve appetite and sleep.
Clinical Evidence
- Preclinical Studies: Animal models of ALS have shown that cannabinoids can extend survival and improve motor function .
- Patient Reports: Many ALS patients report symptom relief with cannabis use, particularly in managing spasticity and pain.
6. Huntington’s Disease (HD)
Overview
Huntington’s disease (HD) is a genetic disorder characterized by the progressive breakdown of nerve cells in the brain, leading to movement, cognitive, and psychiatric disorders.
Cannabinoids and HD
- CBD: May help manage psychiatric symptoms and reduce neuroinflammation.
- THC: Can help alleviate motor symptoms such as chorea (involuntary movements).
Mechanisms of Action
- Neuroprotection: Cannabinoids can protect neurons from damage, potentially slowing disease progression.
- Anti-inflammatory Effects: Reducing neuroinflammation can help manage symptoms and progression of HD.
- Symptom Management: Cannabinoids can alleviate motor and psychiatric symptoms, improving quality of life.
Clinical Evidence
- Clinical Trials: Limited studies suggest that cannabinoids can help manage some symptoms of HD .
- Patient Reports: Anecdotal evidence supports the use of cannabis in managing symptoms such as chorea, anxiety, and depression in HD patients.
Mechanisms of Neuroprotection
Cannabinoids, the active compounds in cannabis, have shown significant promise in protecting neurons and supporting brain health. These neuroprotective mechanisms are multifaceted and involve various biological processes. Understanding these mechanisms is crucial for developing cannabinoid-based therapies for neurological disorders.
1. Reduction of Excitotoxicity
Overview
Excitotoxicity occurs when neurons are damaged and killed by excessive stimulation by neurotransmitters such as glutamate. This process is implicated in various neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis.
Mechanisms
- Glutamate Modulation: Cannabinoids, particularly CBD, can modulate the release of glutamate, reducing excitotoxicity. By decreasing glutamate release, cannabinoids help prevent overstimulation and neuronal damage.
- Calcium Homeostasis: Cannabinoids help regulate calcium influx in neurons. Excessive calcium influx, often triggered by excitotoxicity, can lead to cell death. Cannabinoids reduce calcium entry through voltage-gated calcium channels and N-methyl-D-aspartate (NMDA) receptors.
Evidence
- Preclinical Studies: Animal studies have shown that cannabinoids can reduce glutamate-induced excitotoxicity and protect neurons from damage .
- Clinical Implications: Reducing excitotoxicity can slow the progression of neurodegenerative diseases and mitigate symptoms such as cognitive decline and motor dysfunction.
2. Anti-inflammatory Effects
Overview
Chronic inflammation is a common feature of many neurological disorders. Neuroinflammation can accelerate the development of a disease and worsen neuronal damage.
Mechanisms
- Cytokine Modulation: Cannabinoids, particularly CBD, can modulate the release of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β). This reduces inflammation and protects neurons from inflammatory damage.
- Microglial Activation: Microglia are the immune cells of the CNS. In neurodegenerative diseases, microglia can become overactivated and contribute to neuroinflammation. Cannabinoids can inhibit microglial activation, reducing the release of inflammatory mediators.
- CB2 Receptor Activation: CB2 receptors are primarily located on immune cells. Activation of CB2 receptors by cannabinoids can suppress immune cell activity, reducing inflammation and protecting neural tissue.
Evidence
- Animal Models: Studies in animal models of neurodegenerative diseases have shown that cannabinoids reduce neuroinflammation and improve neuronal survival .
- Human Studies: Preliminary clinical studies suggest that cannabinoids can reduce neuroinflammation in conditions such as multiple sclerosis and Alzheimer’s disease.
3. Antioxidant Properties
Overview
An imbalance between the body’s capacity to eliminate toxic substances through detoxification and the generation of reactive oxygen species (ROS) can lead to oxidative stress. Oxidative stress contributes to neuronal damage and is implicated in various neurological disorders.
Mechanisms
- Free Radical Scavenging: Cannabinoids, particularly CBD, have potent antioxidant properties. They can directly neutralize free radicals, reducing oxidative stress and preventing neuronal damage.
- Regulation of Antioxidant Enzymes: Cannabinoids can upregulate the expression of antioxidant enzymes, such as superoxide dismutase (SOD) and glutathione peroxidase. These enzymes help detoxify ROS and protect neurons from oxidative damage.
- Mitochondrial Protection: Cannabinoids protect mitochondria, the energy-producing organelles in cells, from oxidative damage. By maintaining mitochondrial function, cannabinoids support neuronal health and survival.
Evidence
- Preclinical Studies: Research in animal models has demonstrated that cannabinoids reduce oxidative stress and protect neurons from damage .
- Clinical Implications: Antioxidant properties of cannabinoids may benefit patients with neurodegenerative diseases, traumatic brain injury, and stroke by reducing oxidative damage and improving outcomes.
4. Modulation of Neurotransmitter Systems
Overview
Cannabinoids interact with various neurotransmitter systems, modulating their release and uptake. This modulation can improve symptoms and protect neurons in several neurological disorders.
Mechanisms
- Dopamine Modulation: Cannabinoids can modulate dopamine release, which is critical in conditions such as Parkinson’s disease. By enhancing dopamine signaling, cannabinoids can improve motor function and reduce symptoms such as tremors and rigidity.
- Serotonin Modulation: CBD interacts with serotonin receptors, improving mood and reducing anxiety. This modulation is beneficial in conditions such as anxiety disorders, depression, and PTSD.
- GABAergic System: Cannabinoids enhance the inhibitory effects of the GABAergic system, which helps balance excitatory and inhibitory signals in the brain. This is particularly relevant in epilepsy, where increased inhibition can reduce seizure activity.
Evidence
- Preclinical Studies: Animal studies have shown that cannabinoids modulate neurotransmitter systems, improving symptoms and protecting neurons .
- Clinical Implications: Modulation of neurotransmitter systems by cannabinoids can provide symptomatic relief in various neurological disorders, including epilepsy, Parkinson’s disease, and anxiety disorders.
Challenges and Considerations in the Therapeutic Use of Cannabis for Neurological Disorders
While the potential of cannabis and its constituents, particularly THC and CBD, in treating neurological disorders is promising, several challenges and considerations must be addressed to ensure safe and effective use. These challenges span clinical, regulatory, and practical aspects of cannabis therapy.
1. Lack of Standardization
Overview
One of the primary challenges in the therapeutic use of cannabis is the lack of standardization. This includes variability in cannabis strains, cannabinoid concentrations, and delivery methods.
Issues
- Strain Variability: Different cannabis strains contain varying levels of cannabinoids (THC, CBD) and other compounds (terpenes, flavonoids). This variability can lead to inconsistent therapeutic effects and difficulty in standardizing treatment protocols.
- Dosage and Potency: The concentration of cannabinoids in cannabis products can vary widely, making it challenging to determine the appropriate dosage. Patients may experience different effects based on the potency of the product they use.
- Delivery Methods: There are several ways to consume cannabis, including edibles, oils, vaping, smoking, and topical applications. The rate of absorption and bioavailability of each technique varies, which influences the start and length of the effects.
Solutions
- Standardized Products: Developing standardized cannabis products with consistent cannabinoid concentrations can help ensure reliable therapeutic outcomes. This requires stringent quality control measures during cultivation and production.
- Clear Guidelines: Establishing clear dosing guidelines and protocols based on clinical evidence can help healthcare providers prescribe cannabis more effectively. This includes considering factors such as the patient’s condition, age, weight, and tolerance.
- Research and Education: Continued research into the pharmacokinetics of different delivery methods and educating healthcare providers on these differences can improve the consistency and effectiveness of cannabis therapy.
2. Adverse Effects
Overview
While cannabinoids are generally well-tolerated, they can cause adverse effects, particularly when used in high doses or over long periods.
Issues
- Short-term Effects: Common short-term side effects of THC include dizziness, dry mouth, euphoria, paranoia, and impaired memory and coordination. These effects can be particularly concerning for patients with neurological disorders.
- Long-term Effects: Prolonged use of high-THC cannabis can lead to dependence, cognitive impairment, and psychiatric issues such as anxiety and psychosis. The long-term safety of CBD is generally better, but high doses can cause liver enzyme elevations and drug interactions.
- Interactions with Other Medications: Other drugs and cannabis may interact, changing the medication’s effectiveness or raising the possibility of negative side effects. This is especially important for patients with neurological disorders who often take multiple medications.
Solutions
- Monitoring and Supervision: Close monitoring of patients by healthcare providers can help manage and mitigate adverse effects. This includes regular assessments and adjustments to dosage as needed.
- Patient Education: The chance of negative effects can be decreased by informing patients about possible side effects and how crucial it is to follow recommended dosages. Additionally, patients need to be made aware of the possibility of drug interactions.
- Low-THC and High-CBD Products: Using products with a higher CBD to THC ratio can minimize psychoactive effects and reduce the risk of dependence and cognitive impairment.
3. Legal and Regulatory Issues
Overview
The legal status of cannabis varies widely across different regions, affecting its availability and use for therapeutic purposes.
Issues
- Regulatory Variability: Inconsistent regulations across countries and even within regions of the same country can create confusion and limit access to cannabis-based therapies. This variability affects research, prescription, and distribution.
- Stigma and Perception: Despite growing acceptance, cannabis still faces stigma and negative perceptions, particularly in regions where it remains illegal or is newly legalized. This can discourage patients from seeking cannabis-based treatments and healthcare providers from prescribing them.
- Research Restrictions: Legal restrictions can hinder research on cannabis, limiting the ability to conduct large-scale clinical trials and gather robust evidence on its safety and efficacy.
Solutions
- Harmonized Regulations: Efforts to harmonize regulations at national and international levels can facilitate research, access, and safe use of cannabis-based therapies. This includes standardizing guidelines for cultivation, production, and distribution.
- Public and Professional Education: Educational campaigns targeting the public and healthcare professionals can help reduce stigma and increase awareness of the therapeutic potential of cannabis. This includes providing evidence-based information on the benefits and risks of cannabis use.
- Support for Research: Encouraging and funding research into cannabis through grants and regulatory support can help build the evidence base needed for informed clinical practice and policy decisions.
4. Need for More Research
Overview
Despite the growing body of evidence supporting the therapeutic use of cannabis, more high-quality research is needed to fully understand its potential and limitations.
Issues
- Clinical Trials: Many studies on cannabis are preclinical or observational. There is a need for more randomized controlled trials (RCTs) to establish robust evidence on efficacy, safety, dosing, and long-term effects.
- Mechanisms of Action: While the ECS is well-studied, the specific mechanisms by which cannabinoids exert their therapeutic effects in different neurological disorders require further investigation.
- Patient Populations: More research is needed to understand how different patient populations (e.g., children, elderly, patients with comorbidities) respond to cannabis-based therapies.
Solutions
- Increased Funding: Allocating more resources to cannabis research can support the conduction of large-scale RCTs and other high-quality studies. Governments, private organizations, and academic institutions can play a role in funding this research.
- Collaboration: Collaborative efforts between researchers, healthcare providers, and regulatory bodies can facilitate the design and implementation of comprehensive research studies.
- Long-term Studies: Conducting long-term studies can provide valuable insights into the chronic use of cannabis, its safety profile, and its long-term therapeutic benefits and risks.
5. Patient-Specific Considerations
Overview
The response to cannabis therapy can vary widely among individuals, influenced by factors such as genetics, age, gender, and the presence of other medical conditions.
Issues
- Genetic Variability: Genetic differences can affect how individuals metabolize cannabinoids, leading to variability in therapeutic effects and side effects.
- Age and Gender: Age and gender can influence the pharmacokinetics and pharmacodynamics of cannabinoids, affecting efficacy and safety.
- Comorbidities: Patients with multiple medical conditions may experience different effects from cannabis therapy and are at higher risk for drug interactions.
Solutions
- Personalized Medicine: Adopting a personalized approach to cannabis therapy can help optimize treatment outcomes. This includes genetic testing to understand individual responses to cannabinoids and tailoring dosages accordingly.
- Comprehensive Assessments: Conducting thorough assessments of patients’ medical histories, current medications, and overall health can help identify potential risks and adjust treatment plans accordingly.
- Ongoing Monitoring: Regular monitoring and follow-up can help healthcare providers make necessary adjustments to therapy and address any emerging issues promptly.
Conclusion
The exploration of cannabis and its constituents, particularly THC and CBD, in the treatment of neurological disorders has opened new avenues for therapeutic interventions. The endocannabinoid system (ECS), with its role in regulating various physiological processes, provides a strong foundation for understanding how cannabinoids can modulate neurological functions and offer potential benefits.
Cannabis has shown significant promise in managing conditions such as epilepsy, multiple sclerosis, Parkinson’s disease, Alzheimer’s disease, amyotrophic lateral sclerosis, and Huntington’s disease. The neuroprotective mechanisms of cannabinoids, including the reduction of excitotoxicity, anti-inflammatory effects, antioxidant properties, modulation of neurotransmitter systems, and promotion of neurogenesis, contribute to their therapeutic potential.
However, the therapeutic use of cannabis is not without challenges. The lack of standardization in cannabis products, potential adverse effects, legal and regulatory hurdles, the need for more robust research, and patient-specific considerations are critical factors that need to be addressed to ensure safe and effective treatment outcomes. Standardizing cannabis products, establishing clear dosing guidelines, educating healthcare providers and patients, harmonizing regulations, and fostering research collaborations are essential steps toward overcoming these challenges.
As research continues to evolve, it is crucial to conduct high-quality clinical trials to establish the efficacy and safety of cannabis-based therapies. Personalized approaches to treatment, regular monitoring, and comprehensive patient assessments will further enhance the effectiveness of cannabis in managing neurological disorders.
In conclusion, while there are significant challenges, the potential benefits of cannabis in treating neurological disorders are substantial. By addressing these challenges through research, education, and policy efforts, the medical community can better harness the therapeutic potential of cannabis, offering improved quality of life and symptom management for patients with neurological conditions.