Cannabis and Its Role in Inflammation and Autoimmune Diseases
Cannabis, a plant that has been utilized for thousands of years for medicinal, recreational, and industrial purposes, is now gaining significant attention in modern medicine, particularly in the treatment of inflammation and autoimmune diseases. The therapeutic potential of cannabis is attributed to its complex chemistry, which includes over 100 cannabinoids, with delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most studied. This comprehensive exploration delves into the mechanisms by which cannabis and its constituents influence inflammation and autoimmune conditions, supported by scientific evidence and clinical observations.
Understanding Inflammation and Autoimmune Diseases
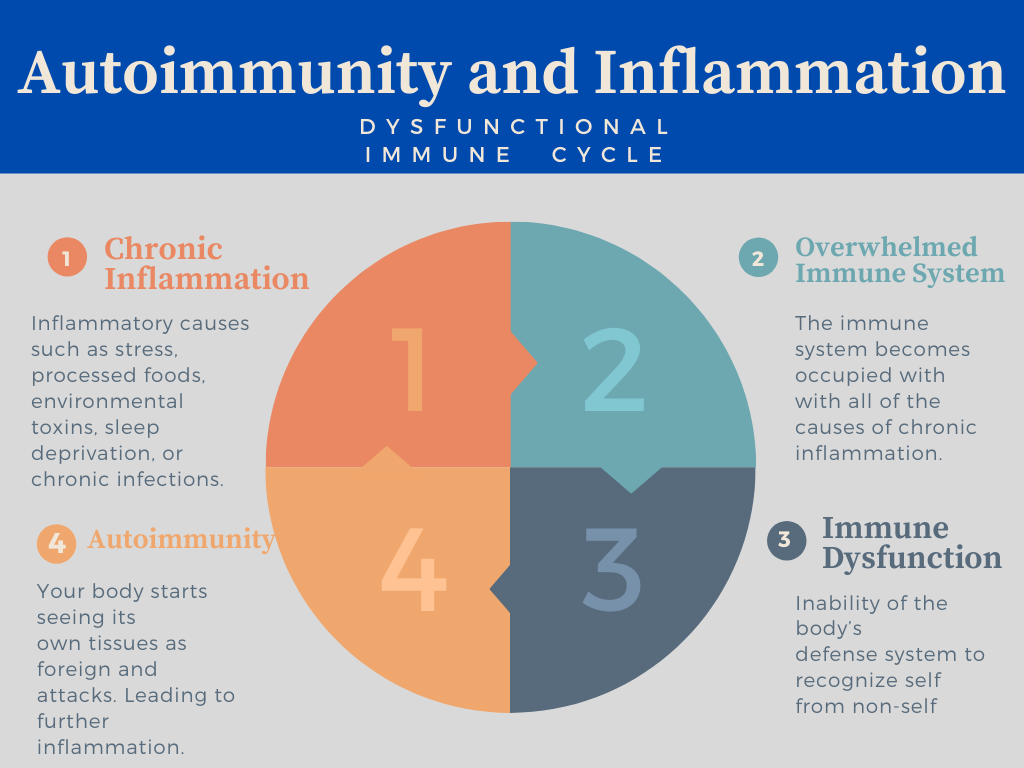
A basic biological reaction to damaging stimuli like infections, damaged cells, or irritants is inflammation. It is a protective mechanism aimed at removing these injurious stimuli and initiating the healing process. On the other hand, autoimmune disorders—diseases in which the body’s own tissues are wrongly attacked by the immune system—can result from persistent inflammation.
Numerous illnesses are classified as autoimmune diseases, such as psoriasis, multiple sclerosis, lupus, rheumatoid arthritis, and inflammatory bowel disease (IBD). Immune system dysregulation, which results in tissue damage and ongoing inflammation, is a hallmark of many disorders.
The Endocannabinoid System
The endocannabinoid system (ECS) plays a crucial role in maintaining homeostasis within the body. It comprises endogenous cannabinoids (endocannabinoids), cannabinoid receptors (CB1 and CB2), and enzymes responsible for the synthesis and degradation of endocannabinoids.
- The central nervous system contains the majority of CB1 receptors, which are important in controlling the release of neurotransmitters.
- The majority of CB2 receptors are found in peripheral tissues, particularly in immune cells, and play a crucial role in controlling inflammation and immunological responses.
Endocannabinoids, such as anandamide (AEA) and 2-arachidonoylglycerol (2-AG), bind to these receptors to exert various physiological effects, including anti-inflammatory actions.
Cannabinoids and Their Anti-Inflammatory Properties
Key Cannabinoids
Cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC) are the two most well-known and researched cannabinoids. Both have demonstrated substantial anti-inflammatory properties, though they work through different mechanisms.
THC (Delta-9-Tetrahydrocannabinol)
Cannabis‘ main psychotropic ingredient is THC. Its actions are mediated through direct binding to cannabinoid receptors, specifically CB1 and CB2 receptors.
- CB2 Receptor Activation: THC’s interaction with CB2 receptors, which are primarily found on immune cells, plays a significant role in its anti-inflammatory effects. Activation of CB2 receptors leads to a reduction in the production of pro-inflammatory cytokines and chemokines, which are signaling molecules that drive the inflammatory response. This results in decreased migration and activation of immune cells at sites of inflammation.
- CB1 Receptor Activation: While CB1 receptors are predominantly located in the central nervous system, their activation also contributes to anti-inflammatory effects. THC binding to CB1 receptors can reduce neuroinflammation, which is particularly relevant in conditions such as multiple sclerosis and neurodegenerative diseases.
CBD (Cannabidiol)
CBD is a non-psychoactive cannabinoid that has gained popularity for its wide range of therapeutic benefits, including its potent anti-inflammatory properties.
- Inhibition of FAAH: The fatty acid amide hydrolase (FAAH) enzyme is inhibited by CBD, preventing it from breaking down the endocannabinoid anandamide. By inhibiting FAAH, CBD increases anandamide levels, which enhances its anti-inflammatory effects through CB2 receptor activation and other mechanisms.
- TRPV1 Activation: CBD activates the transient receptor potential vanilloid 1 (TRPV1) channel, which is involved in pain perception and inflammation. Activation of TRPV1 by CBD can lead to reduced pain and inflammation, contributing to its anti-inflammatory effects.
- PPARγ Activation: CBD activates peroxisome proliferator-activated receptor gamma (PPARγ), a nuclear receptor that regulates genes involved in inflammation and metabolism. Activation of PPARγ by CBD leads to the suppression of inflammatory pathways, further contributing to its anti-inflammatory effects.
Cannabis in Autoimmune Diseases
The potential of cannabis to modulate immune responses and reduce inflammation makes it a promising therapeutic option for autoimmune diseases. Here we explore the evidence supporting the use of cannabis and cannabinoids in specific autoimmune conditions.
Rheumatoid Arthritis (RA)
Rheumatoid arthritis is a chronic inflammatory disorder characterized by synovial inflammation, joint destruction, and systemic manifestations. Conventional treatments include nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs), but these can have significant side effects.
- Preclinical Evidence: Research using arthritic animal models has demonstrated that cannabis help lessen discomfort and inflammation in the joints. THC and CBD have demonstrated efficacy in reducing pro-inflammatory cytokines and immune cell infiltration in joint tissues.
- Clinical Evidence: A randomized controlled trial investigating the efficacy of Sativex (a cannabis-based medicine containing THC and CBD) in patients with rheumatoid arthritis found significant improvements in pain and sleep quality. To validate these results, nevertheless, larger and longer-term investigations are required.
Multiple Sclerosis (MS)
Multiple sclerosis is an autoimmune disease affecting the central nervous system, leading to demyelination, neuroinflammation, and neurodegeneration. Symptoms include muscle spasticity, pain, fatigue, and cognitive impairment.
- Preclinical Evidence: Cannabinoids have shown neuroprotective and anti-inflammatory effects in animal models of MS. They can reduce neuroinflammation, protect against demyelination, and improve motor function.
- Clinical Evidence: Clinical trials have demonstrated that cannabis-based therapies, such as Sativex, can reduce spasticity, pain, and sleep disturbances in MS patients. A systematic review concluded that cannabis-based medicines might be useful as adjunctive treatments for MS-related symptoms.
Inflammatory Bowel Disease (IBD)
Crohn’s disease, ulcerative colitis, and other inflammatory bowel diseases cause the gastrointestinal system to become chronically inflamed, which can cause diarrhea, weight loss, and stomach pain.
- Preclinical Evidence: Animal studies have shown that cannabinoids can reduce intestinal inflammation, decrease cytokine production, and improve gut barrier function in IBD models.
- Clinical Evidence: Observational studies and small clinical trials have reported improvements in IBD symptoms with cannabis use. Patients have reported reduced abdominal pain, improved appetite, and better quality of life. However, more rigorous clinical trials are needed to establish efficacy and safety.
Lupus (Systemic Lupus Erythematosus)
Lupus is a systemic autoimmune disease characterized by widespread inflammation and tissue damage affecting multiple organs, including the skin, joints, kidneys, and brain.
- Preclinical Evidence: Cannabinoids have shown immunosuppressive and anti-inflammatory effects in animal models of lupus. They can reduce autoantibody production, decrease inflammatory cytokines, and protect against organ damage.
- Clinical Evidence: While there is limited clinical research specifically on cannabis use in lupus, anecdotal reports suggest that some patients experience symptom relief with cannabis use. More clinical studies are needed to evaluate its potential benefits.
Psoriasis
Psoriasis is a chronic autoimmune skin disease characterized by hyperproliferation of keratinocytes and inflammation, leading to red, scaly patches on the skin.
- Preclinical Evidence: Cannabinoids have been shown to inhibit keratinocyte proliferation and reduce inflammation in skin models. CBD, in particular, has demonstrated potential in modulating the pathways involved in psoriasis.
- Clinical Evidence: Topical cannabis preparations are increasingly used by patients with psoriasis, with reports of reduced inflammation and itching. However, controlled clinical trials are necessary to validate these observations.
Mechanisms of Action
Cannabinoids exert their therapeutic effects through a variety of mechanisms involving the endocannabinoid system (ECS), other receptor systems, and numerous molecular pathways. Understanding these mechanisms provides insight into how cannabinoids can modulate inflammation and immune responses, offering potential benefits for autoimmune diseases.
1. Modulation of Cytokine Production
Cytokines are signaling proteins that regulate immune and inflammatory responses. Pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukins (IL-1β, IL-6), and interferon-gamma (IFN-γ) play a critical role in the pathogenesis of autoimmune diseases. By regulating these cytokines’ synthesis and release, cannabinoids can lessen inflammation.
- Cannabinoids and Cytokines: Anti-inflammatory cytokines like IL-10 are produced more readily when THC and CBD are present, whereas pro-inflammatory cytokines are suppressed when this occurs. This shift in cytokine balance helps to dampen inflammatory responses and promote tissue healing.
- Mechanisms: The modulation of cytokine production by cannabinoids involves several pathways:
- CB2 Receptor Activation: The release of chemokines and pro-inflammatory cytokines is inhibited when immune cells’ CB2 receptors are activated.
- NF-κB Inhibition: Cannabinoids can inhibit the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, a key regulator of inflammation that controls the expression of many pro-inflammatory cytokines.
- PPARγ Activation: CBD activates peroxisome proliferator-activated receptor gamma (PPARγ), which leads to the suppression of pro-inflammatory genes and the promotion of anti-inflammatory pathways.
2. Regulation of Immune Cell Function
Cannabinoids influence the activity of various immune cells, including T cells, B cells, macrophages, and dendritic cells, which are central to the development and progression of autoimmune diseases.
- T Cells: Cannabinoids modulate T cell responses by:
- Reducing T Cell Proliferation: Cannabinoids can inhibit the proliferation of T cells, thereby reducing the overall immune response.
- Promoting Regulatory T Cells (Tregs): Tregs play a crucial role in maintaining immune tolerance and preventing autoimmune responses. Cannabinoids can promote the development and function of Tregs, which help suppress pathological immune responses.
- Inhibiting Th1 and Th17 Cells: Th1 and Th17 cells are involved in driving autoimmune inflammation. Cannabinoids can inhibit the differentiation and activity of these cells, reducing inflammation.
- B Cells: Cannabinoids can decrease B cell activation and antibody production, which are critical processes in autoimmune diseases such as lupus.
- Macrophages: Cannabinoids influence macrophage polarization:
- M1 to M2 Shift: Macrophages can be changed by cannabinoids from an M1 phenotype that promotes inflammation to an M2 phenotype that inhibits it. M2 macrophages are involved in tissue repair and resolution of inflammation.
- Dendritic Cells: Cannabinoids can inhibit the maturation and antigen-presenting function of dendritic cells, leading to reduced T cell activation and a dampened immune response.
3. Neuroimmune Modulation
The interaction between the nervous system and the immune system, known as neuroimmune crosstalk, plays a significant role in the regulation of inflammation and immune responses. Cannabinoids can modulate this interaction through various mechanisms.
- CB1 Receptors: Activation of CB1 receptors in the central nervous system can modulate the release of neurotransmitters that influence immune function and inflammation. This is particularly relevant in neuroinflammatory conditions such as multiple sclerosis.
- Microglia: The central nervous system’s resident immune cells are called microglia. Cannabinoids can inhibit microglial activation and reduce neuroinflammation, contributing to neuroprotection and the reduction of neuroinflammatory responses.
4. Modulation of Apoptosis and Cell Survival
Apoptosis, or programmed cell death, is a process that helps maintain tissue homeostasis by removing damaged or harmful cells. The pathophysiology of autoimmune disorders may involve dysregulation of apoptosis. Cannabinoids can modulate apoptosis and cell survival pathways.
- Pro-Apoptotic Effects: In certain contexts, cannabinoids can induce apoptosis in immune cells, thereby reducing the number of autoreactive cells that contribute to autoimmune pathology.
- Anti-Apoptotic Effects: In other contexts, cannabinoids can protect cells from apoptosis, promoting cell survival and tissue repair. For example, cannabinoids can protect neuronal cells from apoptosis in neurodegenerative diseases.
5. Modulation of Oxidative Stress
The emergence of inflammation and autoimmune disorders is linked to oxidative stress, which is defined by an imbalance between the generation of reactive oxygen species (ROS) and antioxidant defenses. Cannabinoids have antioxidant properties that can help modulate oxidative stress.
- Reduction of ROS: Cannabinoids can reduce the production of ROS, thereby mitigating oxidative damage to tissues.
- Enhancement of Antioxidant Defenses: Cannabinoids can enhance the activity of endogenous antioxidant systems, helping to protect cells from oxidative stress.
6. Interaction with Other Receptors
In addition to cannabinoid receptors, cannabinoids interact with various other receptors and ion channels that contribute to their anti-inflammatory and immunomodulatory effects.
- TRPV1 Receptors: CBD activates transient receptor potential vanilloid 1 (TRPV1) channels, which are involved in pain perception and inflammation. Activation of TRPV1 by CBD can reduce pain and inflammation.
- GPR55 Receptors: Cannabinoids can interact with G protein-coupled receptor 55 (GPR55), which is involved in modulating inflammation and immune responses.
- Adenosine Receptors: CBD can enhance the signaling of adenosine receptors, which have anti-inflammatory effects.
Safety and Efficacy
The use of cannabis and cannabinoids in treating inflammation and autoimmune diseases raises important considerations regarding safety and efficacy.
Safety Considerations
Psychoactive Effects
- THC: The primary psychoactive component of cannabis, THC, can cause a range of central nervous system effects, including euphoria, anxiety, paranoia, and cognitive impairment. By carefully adjusting the dosage and including CBD, which has calming qualities and can offset some of the euphoric effects of THC, these dose-dependent effects can be lessened.
- CBD: Unlike THC, CBD is non-psychoactive and has a favorable safety profile. High doses of CBD are generally well-tolerated, though some individuals may experience side effects such as dry mouth, diarrhea, reduced appetite, and fatigue.
Drug Interactions
- Cytochrome P450 Enzymes: Both THC and CBD are metabolized by cytochrome P450 enzymes in the liver. Cannabis can interact with other medications that are metabolized by these enzymes, leading to altered drug levels and potential side effects. For example, CBD is known to inhibit CYP3A4 and CYP2D6, which can affect the metabolism of drugs such as warfarin, antiepileptics, and certain antidepressants.
- Pharmacokinetic Interactions: Cannabis can affect the absorption, distribution, metabolism, and excretion of other drugs. It is essential to consider these interactions when combining cannabis with other medications, especially in patients with complex medication regimens.
Long-Term Use
- Tolerance and Dependence: Chronic use of THC can lead to tolerance, where increasing doses are needed to achieve the same effect, and dependence, characterized by withdrawal symptoms upon cessation. While CBD does not produce tolerance or dependence, long-term studies are needed to fully understand the implications of prolonged CBD use.
- Immune System Effects: The long-term effects of cannabis on the immune system are not fully understood. While cannabinoids have immunomodulatory properties that can be beneficial in autoimmune diseases, their impact on immune function over extended periods requires further investigation.
Other Considerations
- Reproductive Health: THC can affect reproductive health, including sperm production and menstrual cycle regulation. Pregnant and breastfeeding women should avoid cannabis use due to potential risks to the developing fetus or infant.
- Mental Health: Individuals with a history of psychiatric disorders, such as schizophrenia or bipolar disorder, may be at increased risk of adverse effects from THC. Careful screening and monitoring are recommended for these populations.
Efficacy Considerations
Individual Variability
- Genetic Factors: Genetic variations can influence individual responses to cannabinoids. For example, polymorphisms in the genes encoding cannabinoid receptors (CNR1 and CNR2) or enzymes involved in cannabinoid metabolism (CYP2C9 and FAAH) can affect the efficacy and safety of cannabinoid therapies.
- Disease Severity and Type: The efficacy of cannabis in treating autoimmune diseases can vary based on the type and severity of the disease. For instance, the benefits observed in rheumatoid arthritis may differ from those in multiple sclerosis or lupus.
Standardization and Dosing
- Dosing Challenges: The lack of standardized dosing and formulations poses challenges in assessing the true efficacy of cannabis. Dosage can vary widely depending on the cannabinoid content, route of administration, and individual patient factors. Personalized dosing regimens are often necessary to achieve optimal therapeutic outcomes.
Clinical Evidence
- Rheumatoid Arthritis: Clinical trials have shown that cannabis-based medicines like Sativex (a combination of THC and CBD) can improve pain and sleep quality in patients with rheumatoid arthritis. Larger, longer-term studies are yet required to validate these results and determine the best dose schedules.
- Multiple Sclerosis: Cannabis-based therapies have demonstrated efficacy in reducing spasticity, pain, and sleep disturbances in MS patients. Systematic reviews suggest that cannabis-based medicines may be beneficial as adjunctive treatments for MS-related symptoms.
- Inflammatory Bowel Disease: Observational studies and small clinical trials have reported improvements in IBD symptoms with cannabis use, including reduced abdominal pain and improved appetite. However, more rigorous clinical trials are needed to establish the efficacy and safety of cannabis in IBD.
- Systemic Lupus Erythematosus: While there is limited clinical research specifically on cannabis use in lupus, anecdotal reports suggest that some patients experience symptom relief with cannabis use. More clinical studies are needed to evaluate its potential benefits and safety.
- Psoriasis: Topical cannabis preparations are increasingly used by patients with psoriasis, with reports of reduced inflammation and itching. Controlled clinical trials are necessary to validate these observations and determine the optimal formulations and dosages.
Combination Therapies
- Adjunctive Use: Cannabis may be most effective when used in combination with other treatments, such as conventional medications, physical therapy, and lifestyle modifications. This integrative approach can enhance therapeutic outcomes and minimize potential side effects.
- Synergistic Effects: The combination of THC and CBD, as seen in products like Sativex, can provide synergistic effects, enhancing the overall efficacy while reducing the psychoactive effects of THC. Further research is needed to explore the potential of combining cannabinoids with other therapeutic agents.
Future Directions
The growing interest in the therapeutic potential of cannabis in inflammation and autoimmune diseases highlights the need for further research to optimize its use.
- Clinical Trials: Well-designed clinical trials are essential to evaluate the safety, efficacy, and optimal dosing of cannabis and cannabinoids in various autoimmune diseases.
- Mechanistic Studies: Understanding the precise molecular mechanisms by which cannabinoids modulate inflammation and immune responses will aid in developing targeted therapies.
- Personalized Medicine: Advances in genomics and personalized medicine could help identify patients who are most likely to benefit from cannabis-based treatments.
- Regulatory Considerations: Regulatory frameworks need to be developed to ensure the quality, safety, and efficacy of cannabis products used for medicinal purposes.
Conclusion
Cannabis and its constituents, particularly the cannabinoids THC and CBD, have emerged as promising therapeutic agents in the management of inflammation and autoimmune diseases. The therapeutic potential of cannabinoids lies in their ability to interact with the endocannabinoid system (ECS) and other molecular pathways to modulate immune responses, reduce inflammation, and alleviate symptoms associated with autoimmune conditions.
Key Points:
- Understanding Inflammation and Autoimmune Diseases: Inflammation is a protective response of the immune system to harmful stimuli, but chronic inflammation can lead to autoimmune diseases, where the immune system mistakenly attacks the body’s own tissues. Lupus, psoriasis, multiple sclerosis, inflammatory bowel disease, and rheumatoid arthritis are examples of common autoimmune illnesses.
- The Endocannabinoid System: The ECS, comprising endocannabinoids, cannabinoid receptors (CB1 and CB2), and enzymes, plays a crucial role in maintaining homeostasis and regulating immune responses. Cannabinoids exert their effects by interacting with this system, influencing various physiological processes.
- Cannabinoids and Their Anti-Inflammatory Properties: THC and CBD, the two most well-known cannabinoids, have demonstrated significant anti-inflammatory and immunomodulatory properties. THC primarily exerts its effects through CB1 and CB2 receptors, while CBD acts through multiple mechanisms, including the inhibition of FAAH, activation of TRPV1 and PPARγ, and modulation of cytokine production.
- Cannabis in Autoimmune Diseases: Cannabinoids have shown potential in managing various autoimmune diseases:
- Rheumatoid Arthritis: Reducing joint inflammation and pain.
- Multiple Sclerosis: Alleviating spasticity, pain, and sleep disturbances.
- Inflammatory Bowel Disease: Improving symptoms and gut barrier function.
- Lupus: Reducing autoantibody production and protecting against organ damage.
- Psoriasis: Inhibiting keratinocyte proliferation and reducing inflammation.
- Mechanisms of Action: The therapeutic effects of cannabinoids are mediated through multiple mechanisms, including modulation of cytokine production, regulation of immune cell function, neuroimmune interactions, modulation of apoptosis and cell survival, reduction of oxidative stress, and interaction with other receptors.
- Safety and Efficacy: The use of cannabinoids requires careful consideration of safety, including psychoactive effects, drug interactions, long-term use, and individual variability. Efficacy can vary based on genetic factors, disease type, and severity. Standardized dosing and formulations, as well as combination therapies, are crucial for optimizing therapeutic outcomes.
- Regulatory and Legal Considerations: The legal status of cannabis varies across regions, impacting research, clinical use, and patient access. Regulatory frameworks are needed to ensure the quality, safety, and efficacy of cannabis products used for medicinal purposes.
- Future Directions: Further research is essential to fully understand the mechanisms of action, optimize dosing regimens, and establish standardized treatment protocols. Well-designed clinical trials, mechanistic studies, advances in personalized medicine, and clear regulatory frameworks will be critical in advancing the therapeutic use of cannabis in autoimmune diseases.
Final Thoughts
Cannabis-based therapies hold significant promise for improving the management of autoimmune diseases and enhancing the quality of life for patients. While challenges remain, the growing body of evidence supports the potential of cannabinoids as valuable additions to the therapeutic arsenal for inflammation and autoimmune conditions. Continued research and clinical advancements will be key to unlocking the full potential of cannabis in medicine, providing safer and more effective treatments for patients worldwide.