
Cannabis and Cancer Treatment Support: An In-Depth Exploration

Cannabis, a plant that has been used for centuries for various medicinal purposes, is gaining increasing attention in modern medicine, particularly in cancer treatment support. This comprehensive exploration delves into the role of cannabis in supporting cancer treatment, its therapeutic potential, mechanisms of action, clinical evidence, and the regulatory landscape.
Introduction
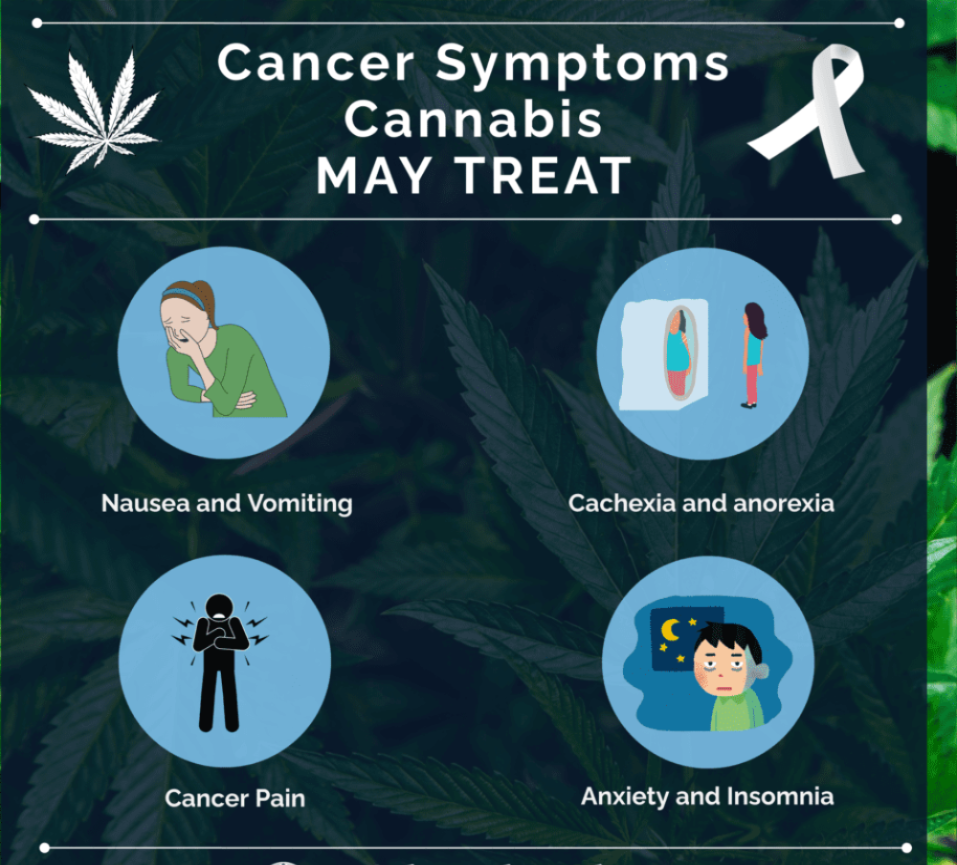
Uncontrolled proliferation and spread of aberrant cells is the hallmark of the complicated disease known as cancer. Traditional cancer treatments, including chemotherapy, radiation, and surgery, often come with severe side effects that significantly impact patients’ quality of life. In recent years, cannabis has emerged as a promising adjunct therapy for managing cancer-related symptoms and side effects, offering a potential improvement in the overall well-being of cancer patients.
The Therapeutic Potential of Cannabis

Tetrahydrocannabinol (THC) and cannabidiol (CBD) are the two most extensively researched of the over 100 cannabinoids found in cannabis. The complex cell-signaling system known as the endocannabinoid system (ECS), which is involved in the regulation of pain, mood, hunger, and immunological response, is influenced by the interactions between these cannabinoids.
1. Pain Management: Pain is a common and often debilitating symptom for cancer patients. Cannabinoids, particularly THC, have been shown to possess analgesic properties. They work by binding to cannabinoid receptors (CB1 and CB2) in the brain and peripheral nervous system, modulating pain perception. Studies have demonstrated that cannabis can provide relief for cancer-related pain, even in cases where traditional pain medications are ineffective.
2. Nausea and Vomiting: Nausea and vomiting are frequent side effects of chemotherapy. Traditional antiemetic drugs may not always be effective, and their use can be limited by side effects. Cannabis, particularly THC, has been shown to be effective in reducing chemotherapy-induced nausea and vomiting (CINV). Cannabis is believed to work through its interactions with serotonin receptors and the ECS to produce its antiemetic effects.
3. Appetite Stimulation: Cancer cachexia, characterized by severe weight loss and muscle wasting, is a serious condition that affects many cancer patients. Cannabis has been found to stimulate appetite, primarily through the action of THC on the CB1 receptors in the brain, which are involved in regulating food intake. This can help improve nutritional intake and body weight in patients suffering from cachexia.
4. Anxiety and Depression: The psychological impact of a cancer diagnosis and treatment can lead to anxiety and depression. CBD, a non-psychoactive cannabinoid, has been found to have anxiolytic and antidepressant properties. It is believed to work through its interaction with serotonin receptors and modulation of the ECS, helping to alleviate anxiety and improve mood in cancer patients.
5. Sleep Disorders: Cancer patients frequently experience sleep problems as a result of pain, worry, and side effects from treatment. It has been demonstrated that THC and CBD both enhance sleep quality. THC may shorten the time it takes to fall asleep and promote deep sleep, while CBD has been shown to enhance the general quality of sleep without producing the “high” that comes with THC.
Mechanisms of Action
The therapeutic effects of cannabis are mediated through its interaction with the ECS, which consists of endocannabinoids, cannabinoid receptors (CB1 and CB2), and enzymes involved in the synthesis and degradation of endocannabinoids.
1. Endocannabinoid System: The body’s equilibrium is preserved in part by the ECS. Anandamide and 2-arachidonoylglycerol (2-AG) are examples of endocannabinoids that bind to CB1 and CB2 receptors to control a variety of physiological activities. The central nervous system has the majority of CB1 receptors, whereas peripheral tissues and the immune system have the majority of CB2 receptors.
2. Cannabinoid Receptors: THC and CBD exert their effects by interacting with CB1 and CB2 receptors. THC is a partial agonist at both receptors, meaning it can activate them to produce physiological responses. Conversely, CBD has a modest affinity for these receptors but has the ability to subtly alter their activity. In addition, CBD has been shown to interact with vanilloid and serotonin receptors, among other receptors, which may account for some of its diverse effects.
3. Enzymes: Enzymes like fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL) are responsible for the breakdown of endocannabinoids. Inhibition of these enzymes can increase endocannabinoid levels, enhancing the activation of CB1 and CB2 receptors. Some cannabinoids, including CBD, have been found to inhibit FAAH and MAGL, contributing to their therapeutic effects.
Clinical Evidence
The clinical evidence supporting the use of cannabis in cancer treatment support is growing, with numerous studies investigating its efficacy and safety in managing various symptoms associated with cancer and its treatments. Below is a detailed examination of the clinical evidence for cannabis in pain management, nausea and vomiting, appetite stimulation, anxiety and depression, and sleep disorders in cancer patients.
Pain Management
Pain is a prevalent and often debilitating symptom in cancer patients, resulting from the disease itself or from treatments like chemotherapy and radiation. Traditional pain medications, including opioids, can be effective but often come with significant side effects and the risk of dependency.
1. Systematic Reviews and Meta-Analyses: A systematic review and meta-analysis published in the Journal of Pain and Symptom Management (2018) assessed the effectiveness of cannabis-based medicines for chronic pain in adults, including cancer pain. The review included 28 studies and found that cannabis-based medicines provided significant pain relief compared to placebo. The authors concluded that cannabis-based medicines might be moderately effective for chronic pain management, with a favorable safety profile compared to opioids.
2. Randomized Controlled Trials (RCTs): Several RCTs have evaluated the efficacy of cannabis in managing cancer-related pain:
- A double-blind, placebo-controlled trial published in The Journal of Pain (2015) investigated the effects of vaporized cannabis in 50 patients with chronic neuropathic pain. The study found that cannabis significantly reduced pain intensity and improved sleep compared to placebo, with a dose-dependent effect.
- Another RCT published in the European Journal of Pain (2018) evaluated the use of an oromucosal spray containing THC and CBD in patients with advanced cancer and refractory pain. The study included 177 patients and found that the cannabis-based spray significantly reduced pain scores and was well-tolerated.
3. Observational Studies: Observational studies provide real-world evidence of the effectiveness of cannabis for cancer pain:
- A large observational study conducted in Israel and published in the European Journal of Internal Medicine (2018) included 2,970 cancer patients who were treated with medical cannabis. The study found that over 95% of patients reported an improvement in their condition, with significant reductions in pain levels and other symptoms.
Nausea and Vomiting
One of the frequent and upsetting side effects of cancer treatment is chemotherapy-induced nausea and vomiting (CINV). While conventional antiemetics can be effective, they are not always sufficient, and some patients experience refractory symptoms.
1. Systematic Reviews and Meta-Analyses: A meta-analysis published in JAMA (2015) reviewed the efficacy of cannabis-based medicines for CINV. The analysis included 28 studies and found that cannabis-based medicines were more effective than conventional antiemetics in reducing nausea and vomiting. The authors noted that patients were more likely to prefer cannabis over traditional antiemetics due to its perceived efficacy and tolerability.
2. Randomized Controlled Trials: Several RCTs have demonstrated the efficacy of cannabis in managing CINV:
- A double-blind, placebo-controlled trial published in The New England Journal of Medicine (2007) evaluated the use of dronabinol (a synthetic form of THC) in patients undergoing chemotherapy. The study found that dronabinol was significantly more effective than placebo in reducing nausea and vomiting.
- Another RCT published in Annals of Oncology (2018) investigated the use of nabilone (a synthetic cannabinoid) in patients with CINV refractory to standard antiemetics. The study included 40 patients and found that nabilone significantly reduced nausea and vomiting compared to placebo.
Appetite Stimulation
Cancer cachexia, characterized by severe weight loss and muscle wasting, is a serious condition that affects many cancer patients. Cannabis has been found to stimulate appetite and improve nutritional intake.
1. Systematic Reviews and Meta-Analyses: A systematic review published in the Cochrane Database of Systematic Reviews (2011) evaluated the effects of cannabis-based medicines on appetite stimulation in cancer patients. The review included 30 studies and found that cannabis-based medicines were associated with significant improvements in appetite and weight gain compared to placebo.
2. Randomized Controlled Trials: RCTs have provided evidence for the appetite-stimulating effects of cannabis:
- A double-blind, placebo-controlled trial published in the Annals of Oncology (2011) assessed the use of THC in patients with advanced cancer and anorexia. The study included 243 patients and found that THC significantly increased appetite and food intake compared to placebo.
- Another RCT published in the Journal of Clinical Oncology (2014) investigated the use of a cannabis extract (containing THC and CBD) in patients with cancer cachexia. The study found that the cannabis extract significantly improved appetite and quality of life compared to placebo.
Anxiety and Depression
A cancer diagnosis and its treatment can have a profound psychological impact that causes worry and sadness. CBD, a non-psychoactive cannabinoid, has been found to have anxiolytic and antidepressant properties.
1. Systematic Reviews and Meta-Analyses: A systematic review published in Neurotherapeutics (2015) reviewed the evidence for the anxiolytic and antidepressant effects of CBD. The review included preclinical and clinical studies and found that CBD has significant potential as a treatment for anxiety and depression, with a favorable safety profile.
2. Randomized Controlled Trials: RCTs have explored the use of CBD for anxiety and depression in cancer patients:
- A double-blind, placebo-controlled trial published in the Brazilian Journal of Psychiatry (2019) evaluated the effects of CBD on anxiety in patients with generalized social anxiety disorder. In comparison to a placebo, the study indicated that CBD dramatically lowered anxiety levels.
- Another RCT published in The Permanente Journal (2019) investigated the use of CBD for anxiety and sleep in a clinical population. The study included 72 patients and found that CBD significantly reduced anxiety scores and improved sleep quality.
Sleep Disorders
Sleep disturbances are common in cancer patients, resulting from pain, anxiety, and treatment side effects. It has been demonstrated that THC and CBD both enhance sleep quality.
1. Systematic Reviews and Meta-Analyses: A systematic review published in Frontiers in Pharmacology (2018) reviewed the evidence for the effects of cannabis on sleep disorders. The review included 29 studies and found that cannabis, particularly THC, was associated with significant improvements in sleep quality and duration.
2. Randomized Controlled Trials: RCTs have demonstrated the efficacy of cannabis in improving sleep in cancer patients:
- A double-blind, placebo-controlled trial published in the Journal of Clinical Oncology (2017) evaluated the use of a cannabis-based medicine (containing THC and CBD) in patients with insomnia related to chronic pain. The study found that the cannabis-based medicine significantly improved sleep quality and reduced insomnia compared to placebo.
- Another RCT published in Sleep (2019) investigated the use of CBD for sleep disturbances in patients with post-traumatic stress disorder (PTSD). The study included 72 patients and found that CBD significantly improved sleep quality and reduced nightmares.
Regulatory Landscape
The legal status of cannabis varies widely across the world, impacting its availability for medical use.
1. United States: In the U.S., cannabis is classified as a Schedule I substance under the Controlled Substances Act, meaning it is considered to have a high potential for abuse and no accepted medical use. However, many states have legalized medical cannabis, allowing its use for various conditions, including cancer. The U.S. Food and Drug Administration (FDA) has approved certain cannabis-based medications, such as dronabinol and nabilone, for CINV.
2. Canada: Canada legalized medical cannabis in 2001 and recreational cannabis in 2018. Health Canada regulates the production and distribution of cannabis, ensuring quality and safety. Medical cannabis is available to patients with a prescription from a healthcare provider, and its use for managing cancer symptoms is well-recognized.
3. Europe: The regulatory landscape for medical cannabis in Europe is diverse. Countries like Germany, Italy, and the Netherlands have established medical cannabis programs, allowing patients to access cannabis for various conditions, including cancer. Other countries have more restrictive regulations, limiting the availability of medical cannabis.
4. Rest of the World: Many countries in South America, such as Brazil and Argentina, have legalized medical cannabis. In Australia, medical cannabis is regulated by the Therapeutic Goods Administration (TGA), and its use for managing cancer symptoms is permitted. In Asia, countries like Thailand and South Korea have recently introduced medical cannabis programs.
Safety and Side Effects
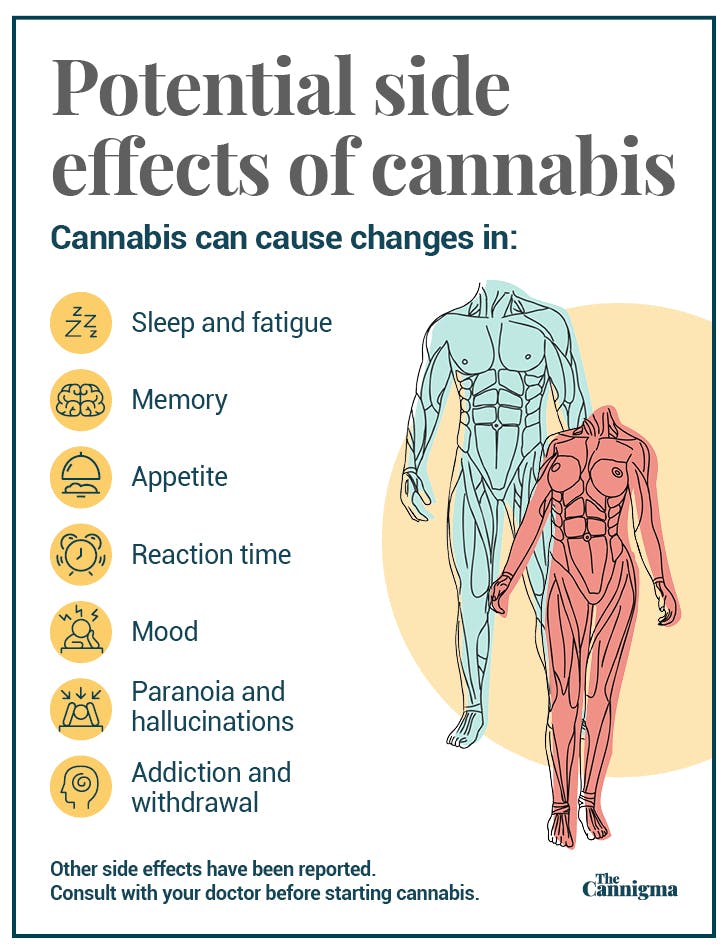
While cannabis offers several potential benefits in managing cancer-related symptoms, it is not without risks. Understanding the safety profile and side effects of cannabis is crucial for both patients and healthcare providers to make informed decisions. This section delves into the various safety considerations and potential side effects associated with the use of cannabis in cancer treatment support.
Psychoactive Effects
1. Euphoria and Cognitive Impairment: The psychoactive component of cannabis, tetrahydrocannabinol (THC), can cause euphoria, altered perception, and cognitive impairment. These effects are dose-dependent and can vary widely among individuals. While some patients may find the euphoric effects beneficial for mood enhancement, others may experience distress, anxiety, or paranoia.
2. Sedation and Dizziness: THC can also induce sedation and dizziness, which may affect daily activities and overall quality of life. Those who take large quantities of cannabis or are new users experience these effects more intensely. To reduce these side effects, patients should be instructed to begin with low doses and increase them gradually as tolerated.
3. Short-Term Memory Impairment: Cannabis use, especially THC-rich strains, can impair short-term memory and attention. This can be particularly concerning for cancer patients who need to manage complex treatment regimens and daily tasks. Patients should be monitored for cognitive effects and provided with strategies to manage potential impairments.
Cardiovascular Effects
1. Heart Rate and Blood Pressure: Cannabis can cause acute changes in cardiovascular function, including increased heart rate (tachycardia) and fluctuations in blood pressure. These effects are primarily mediated by THC and can pose risks for patients with preexisting cardiovascular conditions. Healthcare providers should assess cardiovascular health before recommending cannabis and monitor patients for any adverse effects.
2. Risk of Arrhythmias: There is some evidence to suggest that cannabis use can increase the risk of arrhythmias, particularly in vulnerable populations. Patients with a history of cardiac arrhythmias should use cannabis with caution and under close medical supervision.
Respiratory Effects
1. Smoking-Related Risks: Smoking cannabis can have adverse effects on the respiratory system, similar to those associated with smoking tobacco. These include chronic bronchitis, cough, and an increased risk of respiratory infections. For cancer patients, especially those with compromised respiratory function, smoking cannabis is not recommended.
2. Alternative Delivery Methods: To mitigate respiratory risks, patients can use alternative delivery methods such as vaporization, edibles, tinctures, and oils. By heating the cannabis to a temperature where cannabinoids are released without burning, vaporization lowers the intake of toxic substances. Edibles and tinctures provide a smoke-free option, though they come with their own considerations regarding dosage and onset time.
Drug Interactions
1. Cytochrome P450 Enzyme Interaction: Cannabidiol (CBD) and, to a lesser extent, THC can interact with cytochrome P450 enzymes in the liver, which are responsible for metabolizing many drugs. This interaction can alter the plasma levels of medications, potentially leading to increased side effects or reduced efficacy. Drugs that may be affected include certain chemotherapeutic agents, anticoagulants, antiepileptics, and antidepressants.
2. Monitoring and Dose Adjustments: Patients using cannabis in conjunction with other medications should be closely monitored for potential drug interactions. Healthcare providers may need to adjust dosages of concomitant medications to account for these interactions. Regular blood tests and clinical assessments can help manage and mitigate adverse effects.
Dependency and Withdrawal
1. Risk of Dependency: While the risk of developing dependency on cannabis is lower compared to substances like opioids, it is still a concern, particularly with prolonged use of THC-rich products. Cannabis use disorder (CUD) can develop, characterized by cravings, increased tolerance, and withdrawal symptoms upon cessation.
2. Withdrawal Symptoms: Withdrawal symptoms can include irritability, insomnia, reduced appetite, anxiety, and depression. Supportive care can be used to manage these symptoms, which are typically mild to moderate in nature. Gradual tapering of cannabis use rather than abrupt cessation can help minimize withdrawal symptoms.
Mental Health Effects
1. Anxiety and Paranoia: While cannabis, particularly CBD, can have anxiolytic effects, THC can induce or exacerbate anxiety and paranoia in some individuals. This is especially true for patients who consume high doses of THC or who have a predisposition to anxiety disorders.
2. Psychosis: High doses of THC have been associated with transient psychotic episodes, particularly in individuals with a history of psychiatric disorders or those predisposed to psychosis. Patients with a history of mental health issues should use cannabis with caution and under medical supervision.
Gastrointestinal Effects
1. Gastrointestinal Distress: Cannabis use, especially in edible form, can sometimes cause gastrointestinal distress, including nausea, vomiting, and diarrhea. These effects are typically dose-related and can be managed by adjusting the dosage or switching to a different delivery method.
2. Appetite Changes: While THC is known for its appetite-stimulating effects, CBD can have the opposite effect in some individuals, potentially reducing appetite. This dual effect should be considered when recommending cannabis for appetite stimulation in cancer patients.
Long-Term Health Effects
1. Cognitive and Behavioral Effects: Long-term cannabis use, particularly starting in adolescence, has been associated with cognitive and behavioral changes. However, the relevance of these findings to cancer patients, who are typically older and using cannabis for symptom management rather than recreational purposes, is less clear. Continued research is needed to understand the long-term health effects of medical cannabis use in cancer patients.
2. Immune System Modulation: Cannabis has immunomodulatory effects, which could theoretically impact cancer progression and response to treatment. However, current evidence is inconclusive, and more research is needed to determine the implications of long-term cannabis use on the immune system and cancer outcomes.
Future Directions and Research
The potential of cannabis in cancer treatment support is an evolving field of research. Several areas warrant further investigation to optimize its use and maximize its benefits for cancer patients.
1. Clinical Trials: More high-quality clinical trials are needed to establish the efficacy and safety of cannabis for various cancer-related symptoms. These trials should focus on determining optimal dosages, treatment protocols, and long-term effects.
2. Cannabinoid Formulations: Research into different cannabinoid formulations, such as THC
ratios and other cannabinoids like cannabigerol (CBG) and cannabinol (CBN), can help tailor treatments to individual patient needs. Understanding the synergistic effects of cannabinoids, known as the entourage effect, can lead to more effective therapies.
3. Personalized Medicine: The most probable patients to benefit from cannabis-based medicines can be identified with the aid of genetics and personalized medicine advancements. Genetic factors, such as variations in cannabinoid receptor genes, can influence individual responses to cannabis.
4. Mechanisms of Action: Further research into the mechanisms of action of cannabinoids can provide insights into their therapeutic potential. Understanding how cannabinoids interact with the ECS and other signaling pathways can lead to the development of targeted therapies.
5. Education and Training: Healthcare providers need education and training on the use of cannabis for cancer treatment support. This includes understanding the pharmacology of cannabinoids, potential side effects, and legal considerations. Providing accurate and evidence-based information can help healthcare providers guide patients in making informed decisions.
Summary
Cannabis has emerged as a significant adjunct therapy in the management of cancer-related symptoms, offering potential relief for pain, nausea and vomiting, appetite loss, anxiety, depression, and sleep disturbances. The growing body of clinical evidence supports the efficacy of cannabis-based treatments in improving the quality of life for cancer patients. The therapeutic benefits of cannabis are largely attributed to its interaction with the endocannabinoid system, which plays a crucial role in regulating various physiological processes.
Therapeutic Potential
There are many cannabinoids in cannabis, but the most researched are THC and CBD. These compounds interact with the body’s and brain’s cannabinoid receptors to provide a range of medicinal effects.
- Pain Management: Cannabinoids have demonstrated significant analgesic properties, providing relief for cancer-related pain even in cases where traditional pain medications fail.
- Nausea and Vomiting: Cannabis, particularly THC, has proven effective in reducing chemotherapy-induced nausea and vomiting, offering an alternative when conventional antiemetics are insufficient.
- Appetite Stimulation: THC’s ability to stimulate appetite can help combat cancer cachexia, improving nutritional intake and body weight in patients.
- Anxiety and Depression: CBD has shown anxiolytic and antidepressant effects, helping alleviate the psychological burden of cancer.
- Sleep Disorders: It has been discovered that THC and CBD both enhance the quality of sleep, treating insomnia and other sleep disorders that are typical in cancer patients.
Mechanisms of Action
The endocannabinoid system (ECS) is central to the therapeutic effects of cannabis. The ECS consists of cannabinoid receptors (CB1 and CB2), endocannabinoids, and enzymes that regulate their synthesis and degradation. THC predominantly functions as a partial agonist at CB1 and CB2 receptors, but CBD interacts with other receptors, including serotonin and vanilloid receptors, and indirectly modifies the activity of these receptors.
Clinical Evidence
A substantial amount of clinical research supports the use of cannabis in cancer treatment support:
- Pain Management: Systematic reviews and randomized controlled trials (RCTs) have shown cannabis to be effective in reducing cancer-related pain.
- Nausea and Vomiting: Meta-analyses and RCTs indicate that cannabis-based medicines are superior to conventional antiemetics for chemotherapy-induced nausea and vomiting.
- Appetite Stimulation: Clinical trials have demonstrated THC’s efficacy in increasing appetite and food intake in cancer patients.
- Anxiety and Depression: Studies highlight CBD’s potential in reducing anxiety and improving mood.
- Sleep Disorders: Evidence supports the use of cannabis, particularly THC and CBD, in improving sleep quality for cancer patients.
Safety and Side Effects
Cannabis is not risk-free, despite its possible advantages. Safety considerations include:
- Psychoactive Effects: THC can cause euphoria, dizziness, and cognitive impairment.
- Cardiovascular Effects: Cannabis can affect heart rate and blood pressure, posing risks for patients with cardiovascular conditions.
- Respiratory Effects: Smoking cannabis can harm the respiratory system; alternative delivery methods like vaporization and edibles are recommended.
- Drug Interactions: Cannabis can interact with other medications, necessitating careful monitoring.
- Dependency and Withdrawal: Long-term use can lead to dependency and withdrawal symptoms, though the risk is lower compared to opioids.
- Mental Health Effects: High doses of THC can induce anxiety, paranoia, and psychosis in predisposed individuals.
Regulatory Landscape
The legal status of cannabis varies globally, affecting its accessibility for medical use. In many regions, regulatory frameworks ensure the quality and safety of medical cannabis products. However, in areas with restrictive regulations, patients may resort to unregulated sources, posing additional risks.
Future Directions
Further research is needed to optimize the use of cannabis in cancer treatment support. Areas of interest include:
- Clinical Trials: High-quality trials to establish optimal dosages, treatment protocols, and long-term effects.
- Cannabinoid Formulations: Exploring different cannabinoid combinations and their synergistic effects.
- Personalized Medicine: Identifying genetic factors that influence individual responses to cannabis.
- Mechanisms of Action: Understanding how cannabinoids interact with the ECS and other signaling pathways.
- Education and Training: Providing healthcare providers with the necessary knowledge to guide patients in the safe and effective use of cannabis.
Conclusion
Cannabis holds significant promise as a supportive therapy for cancer treatment, offering potential benefits in managing pain, nausea, appetite loss, anxiety, depression, and sleep disturbances. However, given the possible hazards and adverse consequences, using it should be done so with caution. Sustained investigation and clinical trials are necessary to confirm the effectiveness, safety, and ideal application of cannabis in the support of cancer treatment. As the regulatory landscape evolves, ensuring access to safe and effective cannabis-based therapies, guided by evidence-based medical practice, is crucial for improving the quality of life for cancer patients.