
Can Cannabis Increase Appetite in Cancer Patients? A Comprehensive Analysis
Introduction
For thousands of years, people have utilized cannabis, sometimes referred to as marijuana, for medical purposes. In recent decades, its potential therapeutic benefits have gained renewed interest, particularly in the field of oncology. One of the most promising areas of research is the use of cannabis to increase appetite in cancer patients. This paper explores the mechanisms by which cannabis can enhance appetite, the evidence supporting its use, potential risks, and practical considerations for implementation.
Understanding Cancer-Related Anorexia and Cachexia
Cancer-related anorexia and cachexia are severe conditions that affect a significant number of cancer patients. Anorexia is characterized by a loss of appetite, while cachexia is a complex syndrome involving weight loss, muscle wasting, and a decline in physical function. Both conditions are associated with poor prognosis and reduced quality of life.
Mechanisms of Cancer-Related Anorexia and Cachexia
Cancer and its treatments can disrupt normal metabolic processes, leading to anorexia and cachexia. Tumor growth can produce inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which interfere with appetite regulation and metabolism. Additionally, chemotherapy and radiation can cause nausea, vomiting, and taste alterations, further reducing food intake.
The Role of the Endocannabinoid System in Appetite Regulation
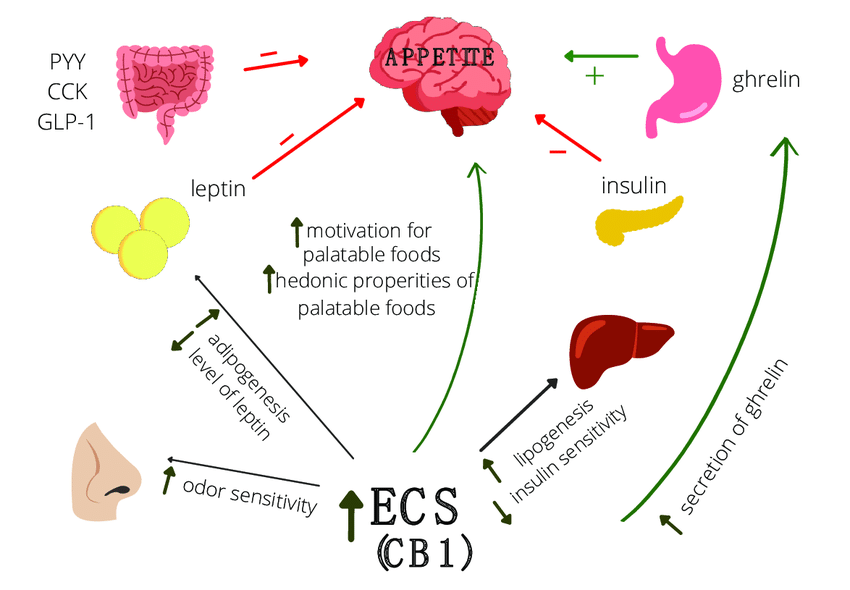
The regulation of hunger, energy balance, and metabolism is significantly influenced by the endocannabinoid system (ECS). Endocannabinoids, receptors, and enzymes make up the ECS. The primary receptors involved in appetite regulation are CB1 and CB2 receptors, which are activated by endocannabinoids such as anandamide and 2-arachidonoylglycerol (2-AG).
CB1 Receptors and Appetite Stimulation
CB1 receptors are predominantly located in the central nervous system, including areas of the brain that control appetite and food intake. Activation of CB1 receptors by endocannabinoids or exogenous cannabinoids like THC (tetrahydrocannabinol) can stimulate appetite.
Evidence Supporting the Use of Cannabis for Appetite Stimulation in Cancer Patients
Cannabis has been increasingly recognized for its potential to stimulate appetite and manage cachexia (wasting syndrome) in cancer patients. Several studies and clinical trials have investigated the efficacy and safety of cannabis and its derivatives, providing a substantial body of evidence that supports its use in this context. This section outlines key findings from clinical trials, observational studies, and reviews to highlight the role of cannabis in appetite stimulation for cancer patients.
Clinical Trials and Studies
- Dronabinol (Synthetic THC) Studies
- Study 1: A randomized, double-blind, placebo-controlled trial evaluated the effects of dronabinol on appetite and weight in cancer patients. The study found that patients receiving dronabinol reported a significant increase in appetite and caloric intake compared to those receiving a placebo. Additionally, some patients experienced modest weight gain.
- Study 2: Another study compared the effects of dronabinol and megestrol acetate, a common appetite stimulant, in cancer patients. While both drugs improved appetite and weight, dronabinol also provided additional benefits in mood and quality of life, suggesting its multifaceted therapeutic potential.
- Nabilone (Synthetic Cannabinoid) Studies
- Study 1: A clinical trial assessed the efficacy of nabilone in improving appetite and reducing nausea in cancer patients. Results indicated that nabilone significantly enhanced appetite and food intake, while also reducing nausea and vomiting associated with chemotherapy.
- Study 2: In a crossover study, nabilone was compared to a placebo in advanced cancer patients. Patients reported better appetite, less nausea, and improved overall well-being when taking nabilone, highlighting its potential as a supportive care medication in oncology.
- Cannabis Extracts (THC and CBD) Studies
- Study 1: A pilot study investigated the use of a cannabis extract containing both THC and CBD in patients with cancer-related cachexia. Participants reported improvements in appetite, sleep, and quality of life. The combination of THC and CBD appeared to offer synergistic benefits, enhancing the therapeutic effects while potentially mitigating some of the psychoactive side effects of THC alone.
- Study 2: A randomized controlled trial evaluated the effects of a cannabis extract (THC
) versus placebo in patients with advanced cancer. The study found significant improvements in appetite and overall quality of life in the cannabis group compared to the placebo group, suggesting a promising role for cannabis extracts in managing cancer-related symptoms.
Observational Studies and Patient Reports
- Observational Study 1: A large-scale observational study involving cancer patients using medical cannabis for symptom management reported that a significant proportion of patients experienced improved appetite and weight stabilization. Patients also noted reductions in pain, nausea, and anxiety, contributing to better overall well-being.
- Patient Reports and Case Studies: Numerous case reports and patient testimonials highlight the positive impact of cannabis on appetite and food intake. Patients often describe a noticeable increase in hunger and enjoyment of food, which can be particularly beneficial in counteracting the anorexia associated with cancer and its treatments.
Mechanisms of Appetite Stimulation by Cannabis

Cannabis, particularly its psychoactive component THC (tetrahydrocannabinol), is well-known for its appetite-stimulating effects, commonly referred to as “the munchies.” The mechanisms through which cannabis stimulates appetite involve a complex interplay between the endocannabinoid system (ECS) and various physiological processes in the body. This section delves into the key mechanisms by which cannabis enhances appetite, including the direct stimulation of CB1 receptors, modulation of neurotransmitters, reduction of nausea and vomiting, and improvement of mood and stress.
Direct Stimulation of CB1 Receptors
The control of hunger, energy balance, and metabolism is entirely dependent on the ECS. The cannabinoid receptors, specifically the CB1 and CB2 receptors, are essential to this system. The central nervous system, which includes the limbic system and hypothalamus, two parts of the brain involved in controlling appetite, is home to the majority of CB1 receptors.
- Hypothalamic Regulation
- The hypothalamus plays a critical role in hunger and satiety signaling. Activation of CB1 receptors in the hypothalamus stimulates the release of orexigenic peptides, such as neuropeptide Y (NPY) and agouti-related peptide (AgRP), which promote food intake and reduce energy expenditure.
- CB1 receptor activation inhibits anorexigenic peptides like pro-opiomelanocortin (POMC) and cocaine- and amphetamine-regulated transcript (CART), which suppress appetite and increase energy expenditure. This dual action of promoting hunger signals and suppressing satiety signals leads to an overall increase in appetite.
- Limbic System
- The limbic system, particularly the nucleus accumbens, is associated with the reward and pleasure aspects of eating. Activation of CB1 receptors in the nucleus accumbens enhances the release of dopamine, a neurotransmitter that promotes the rewarding sensation of eating. This makes food more appealing and enjoyable, further stimulating appetite.
Modulation of Neurotransmitters
Cannabis influences the release and activity of various neurotransmitters involved in appetite regulation, mood, and reward.
- Dopamine
- Cannabis, through the activation of CB1 receptors, increases the release of dopamine in the brain’s reward pathways. Dopamine is crucial for the motivation and pleasure associated with eating, thereby enhancing the desire to eat.
- Serotonin
- Serotonin is another neurotransmitter involved in appetite and mood regulation. While serotonin generally suppresses appetite, the interaction between cannabinoids and serotonin pathways can modulate appetite and mood in complex ways. For example, CBD (cannabidiol) may influence serotonin receptors, contributing to a balanced appetite and mood.
- GABA and Glutamate
- Cannabis also affects the balance between excitatory (glutamate) and inhibitory (GABA) neurotransmitters in the brain. This balance is crucial for maintaining overall neural function and can influence appetite regulation indirectly by affecting mood and stress levels.
Reduction of Nausea and Vomiting
One of the significant barriers to adequate food intake in cancer patients is nausea and vomiting, often induced by chemotherapy and radiation therapy. Cannabis, particularly THC, has potent antiemetic properties that can alleviate these symptoms.
- Central Mechanisms
- THC acts on the brainstem, particularly the dorsal vagal complex, which is involved in the control of vomiting. By binding to CB1 receptors in this region, THC can reduce the activity of the vomiting center, thereby preventing nausea and vomiting.
- Peripheral Mechanisms
- CB1 receptors are also present in the gastrointestinal tract, where they can modulate gut motility and reduce nausea. By decreasing the gastrointestinal tract’s hyperactivity, cannabis can make food intake more comfortable for patients experiencing treatment-related gastrointestinal disturbances.
Improvement of Mood and Stress
Cancer and its treatments can lead to significant psychological distress, including anxiety, depression, and stress, all of which can negatively impact appetite. Cannabis has anxiolytic (anxiety-reducing) and antidepressant properties that can improve mood and reduce stress, indirectly promoting a healthier appetite.
- Anxiolytic Effects
- Cannabinoids, especially CBD, have been shown to reduce anxiety by interacting with serotonin receptors and modulating the brain’s stress response. Lowering anxiety can help patients feel more relaxed and willing to eat.
- Antidepressant Effects
- The mood-enhancing effects of cannabinoids can combat depression, a common issue in cancer patients. Improved mood can increase interest in food and eating, contributing to better nutritional intake.
- Stress Reduction
- Chronic stress can suppress appetite through the release of stress hormones like cortisol. By modulating the ECS and reducing the body’s stress response, cannabis can help normalize appetite and food intake.
Potential Risks and Side Effects of Cannabis Use in Cancer Patients

While cannabis has shown potential benefits in stimulating appetite and managing symptoms in cancer patients, it is not without risks and side effects. In order to make educated judgments regarding the use of cannabis in cancer therapy, patients and healthcare professionals must be aware of these possible drawbacks.
Psychoactive Effects
The primary psychoactive component of cannabis, THC (tetrahydrocannabinol), can cause various mental and cognitive effects, which may not be desirable, especially in vulnerable populations.
- Euphoria and Altered Perception
- THC has the ability to produce elevated mood, altered sensory perception, and euphoric sensations. While some patients might find these effects pleasant, others may experience discomfort or dysphoria.
- Cognitive Impairment
- Excessive THC dosages can affect executive function, short-term memory, and concentration. Patients who are elderly or have pre-existing cognitive problems should be especially concerned about this.
- Anxiety and Paranoia
- Some individuals may experience increased anxiety, paranoia, or panic attacks, especially with high doses of THC or in individuals with a predisposition to anxiety disorders.
Cardiovascular Effects
Cannabis can influence cardiovascular function, posing risks, particularly for patients with existing heart conditions.
- Tachycardia
- THC can cause an increase in heart rate, which might be problematic for patients with arrhythmias or other cardiovascular diseases.
- Hypotension
- Cannabis can lead to orthostatic hypotension (a sudden drop in blood pressure upon standing), causing dizziness or fainting, which can be hazardous for cancer patients with frailty or mobility issues.
- Cardiac Events
- There is some evidence suggesting a potential risk of acute coronary syndromes, such as myocardial infarction (heart attack), in susceptible individuals after cannabis use, particularly in those with a history of heart disease.
Respiratory Issues
Smoking cannabis, a common method of administration, can lead to respiratory problems.
- Chronic Bronchitis
- Regular smoking of cannabis can cause chronic bronchitis, characterized by persistent cough, sputum production, and airway inflammation.
- Lung Infections
- Immunocompromised cancer patients may be at increased risk of lung infections due to the inhalation of potentially harmful microorganisms and irritants present in cannabis smoke.
- Alternative Methods
- To mitigate these risks, alternative administration methods such as vaporization, edibles, tinctures, or capsules are recommended. These methods bypass the harmful effects of smoking while still delivering the therapeutic benefits of cannabis.
Interaction with Other Medications
Cannabis can interact with various medications, potentially altering their effectiveness and safety profiles.
- Cytochrome P450 Enzymes
- Many medicines are metabolized by the liver’s cytochrome P450 enzymes, which can be inhibited by cannabis, especially CBD. The drugs that these enzymes digest may become more concentrated as a result of this interaction, and they may even become hazardous.
- Warfarin and Anticoagulants
- Cannabis can potentiate the effects of anticoagulants like warfarin, increasing the risk of bleeding. Close monitoring and potential dose adjustments are necessary when these drugs are used concurrently.
- Chemotherapy Agents
- Interactions with chemotherapy drugs can alter their metabolism and efficacy. Oncologists must carefully consider potential interactions and monitor for adverse effects when patients use cannabis alongside chemotherapy.
Dependence and Withdrawal
Chronic use of cannabis can lead to psychological dependence and withdrawal symptoms upon cessation.
- Psychological Dependence
- Regular use of cannabis can lead to psychological dependence, characterized by cravings and continued use despite adverse consequences.
- Withdrawal Symptoms
- Withdrawal symptoms can include irritability, insomnia, decreased appetite, anxiety, and mood swings. These symptoms can complicate the clinical management of cancer patients, particularly those with a history of substance use disorders.
- Tapering and Support
- Gradual tapering of cannabis use and psychological support can help manage withdrawal symptoms and reduce the risk of dependence.
Practical Considerations for Implementing Cannabis Therapy
Implementing cannabis therapy for cancer patients involves a careful and strategic approach to ensure safety, efficacy, and compliance with legal regulations. This section outlines key practical considerations for healthcare providers and patients when incorporating cannabis into cancer care, including patient selection, dosage and administration, legal and regulatory issues, and monitoring and follow-up.
Patient Selection
Not all cancer patients are suitable candidates for cannabis therapy. Careful patient selection is crucial to maximize benefits and minimize risks.
- Medical History and Comorbidities
- Review the patient’s medical history, focusing on conditions that might be exacerbated by cannabis use, such as cardiovascular disease, psychiatric disorders, or a history of substance abuse.
- Evaluate the patient’s current medications to identify potential interactions with cannabis.
- Age and Vulnerability
- Consider the patient’s age, as elderly patients may be more susceptible to the psychoactive effects of THC and potential cognitive impairment.
- Assess frailty and overall health status to determine if the patient can tolerate potential side effects.
- Cancer Type and Stage
- Understand the type and stage of cancer, as some cancers may respond better to cannabis therapy than others.
- Evaluate the symptoms the patient is experiencing, such as pain, nausea, and anorexia, to tailor the cannabis treatment to their specific needs.
Dosage and Administration
For cannabis therapy to be both safe and effective, the right dosage and delivery route must be chosen.
- Starting Low and Going Slow
- Begin with a low dose of cannabis and gradually increase it under medical supervision to minimize side effects and find the optimal therapeutic dose.
- Adjust the dosage based on the patient’s response, symptom relief, and any adverse effects.
- Forms of Cannabis
- Inhalation (Smoking or Vaporization): Provides rapid onset of effects but may cause respiratory issues. Vaporization is preferred over smoking to reduce harmful byproducts.
- Oral (Edibles, Capsules, Tinctures): Offers longer-lasting effects but has a delayed onset. Dosing can be more challenging due to variability in absorption and metabolism.
- Sublingual (Tinctures, Sprays): Provides relatively rapid onset and easy dosage control.
- Topical (Creams, Ointments): Useful for localized pain relief but not effective for systemic symptoms like nausea or appetite loss.
- THC and CBD Ratios
- Determine the appropriate ratio of THC to CBD based on the patient’s needs and tolerance. THC is more effective for appetite stimulation and pain relief, while CBD can mitigate some of THC’s psychoactive effects and provide additional anti-inflammatory and anxiolytic benefits.
- Products with varying THC
ratios are available, allowing for tailored treatment plans.
Legal and Regulatory Considerations
The legal status of cannabis varies by jurisdiction, and healthcare providers must ensure compliance with local laws and regulations.
- State and Federal Laws
- Learn about the laws governing medicinal marijuana in your area, including any limitations on its possession, use, and distribution.
- Ensure that cannabis is obtained from licensed and reputable sources to guarantee product quality and safety.
- Medical Cannabis Programs
- Enroll patients in state or national medical cannabis programs if required, which may involve obtaining a medical cannabis card or prescription from a certified physician.
- Familiarize yourself with the program’s regulations, including documentation and reporting requirements.
- Patient Education
- Educate patients about the legal aspects of using cannabis, including safe storage and transport.
- Discuss potential workplace and driving implications, as cannabis use can affect cognitive and motor functions.
Monitoring and Follow-Up
In order to guarantee the safe and efficient use of cannabis therapy in cancer patients, routine monitoring and follow-up are crucial.
- Assessment of Efficacy and Side Effects
- Schedule regular follow-up appointments to assess the efficacy of cannabis therapy in relieving symptoms such as pain, nausea, and appetite loss.
- Monitor for potential side effects, including cognitive impairment, anxiety, and cardiovascular effects.
- Adjustments to Treatment
- Adjust the dosage and administration method based on the patient’s response and any adverse effects. This may involve switching from one form of cannabis to another or altering the THC
ratio. - Be prepared to discontinue cannabis therapy if the risks outweigh the benefits or if the patient experiences significant side effects.
- Adjust the dosage and administration method based on the patient’s response and any adverse effects. This may involve switching from one form of cannabis to another or altering the THC
- Patient Support and Counseling
- Provide ongoing support and counseling to address any concerns or issues related to cannabis use, including managing expectations and addressing psychological dependence.
- Urge patients to report right away any new symptoms or modifications to their condition.
Conclusion
Cannabis therapy has emerged as a promising approach for managing appetite stimulation and cachexia in cancer patients. Because the endocannabinoid system is essential for controlling hunger, energy balance, and metabolism, cannabis’s medicinal promise is supported by its capacity to interact with this system. The mechanisms through which cannabis stimulates appetite include the direct activation of CB1 receptors, modulation of neurotransmitters, reduction of nausea and vomiting, and improvement of mood and stress.
Clinical evidence supports the efficacy of cannabis and its derivatives, such as THC and CBD, in increasing appetite and improving the quality of life for cancer patients. Numerous studies, including randomized controlled trials and observational studies, have demonstrated that cannabis can enhance appetite, reduce chemotherapy-induced nausea and vomiting, and provide additional benefits such as pain relief and mood improvement. However, the use of cannabis in cancer therapy is not without risks and side effects, which include psychoactive effects, cardiovascular concerns, respiratory issues, potential drug interactions, and the risk of dependence and withdrawal.
Implementing cannabis therapy in cancer care requires a thoughtful and comprehensive approach. Healthcare providers must carefully select suitable patients, consider individual medical histories, and be mindful of potential interactions with other medications. Starting with low doses and gradually increasing under medical supervision is essential to minimize side effects and determine the optimal therapeutic dose. Additionally, the legal and regulatory landscape surrounding cannabis varies by jurisdiction, necessitating compliance with local laws and guidelines.
Regular monitoring and follow-up are critical to assess the efficacy and safety of cannabis therapy. This includes evaluating symptom relief, adjusting dosages, and addressing any adverse effects or concerns from patients. Educating patients about the legal, safety, and practical aspects of cannabis use is also crucial for ensuring informed and responsible use.
In conclusion, while cannabis holds significant promise for increasing appetite and managing symptoms in cancer patients, it is essential to balance the potential benefits with the associated risks. Continued research and clinical trials are necessary to further elucidate the mechanisms, optimize dosing strategies, and enhance the therapeutic application of cannabis in oncology. By adopting a patient-centered approach and adhering to best practices, healthcare providers can effectively integrate cannabis therapy into cancer care, offering hope and relief to many patients and their families.